

Background: There is emerging evidence of a relationship between psoriasis and metabolic syndrome, increased prevalence of cardiovascular risk factors and adverse cardiovascular outcomes. Obesity is a risk factor for psoriatic disease itself but there has been less emphasis on body mass alterations and the distribution between separate compartments: fat-free tissue (lean body mass), extracellular water and adipose tissue. Body composition is a term used to describe the percentages of fat, bone, water and muscle in human bodies and is an emerging tool in assessment of physical fitness and metabolic health, although its role in disease is less well appreciated.
Objectives: To identify whether psoriatic patients, including those with psoriatic arthritis, confer specific and recognizable body composition changes compared with the general population, and to review existing modalities for the assessment of body composition.
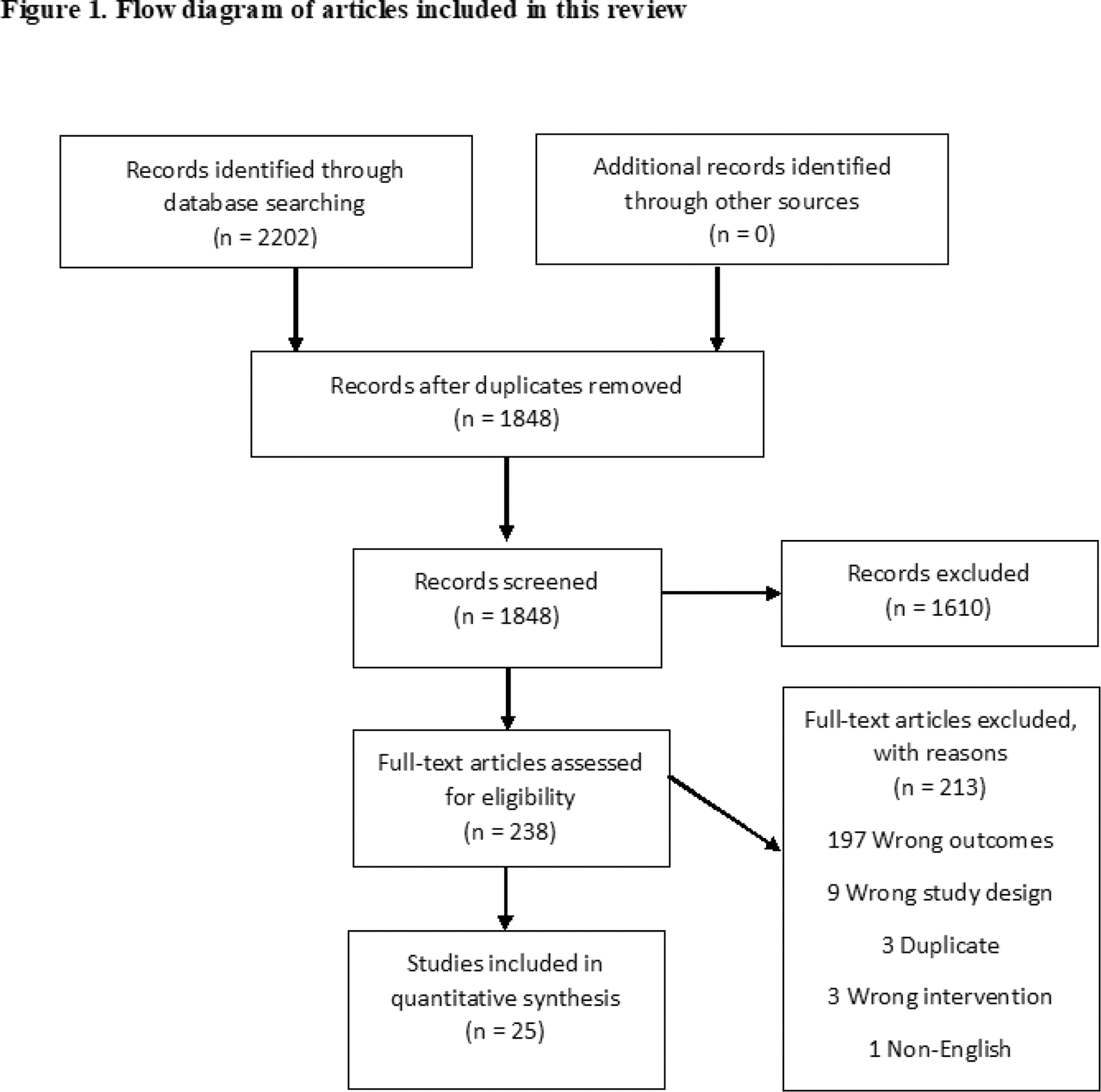
Methods: Electronic searches of the literature were conducted in PubMed, Medline (Ovid ® ), Embase (Ovid ® ), Cochrane Central Register and Google Scholar. Titles and abstracts were reviewed by two authors independently against a set of prespecified inclusion/exclusion criteria, reference lists were examined and synthesis of the included studies was conducted.
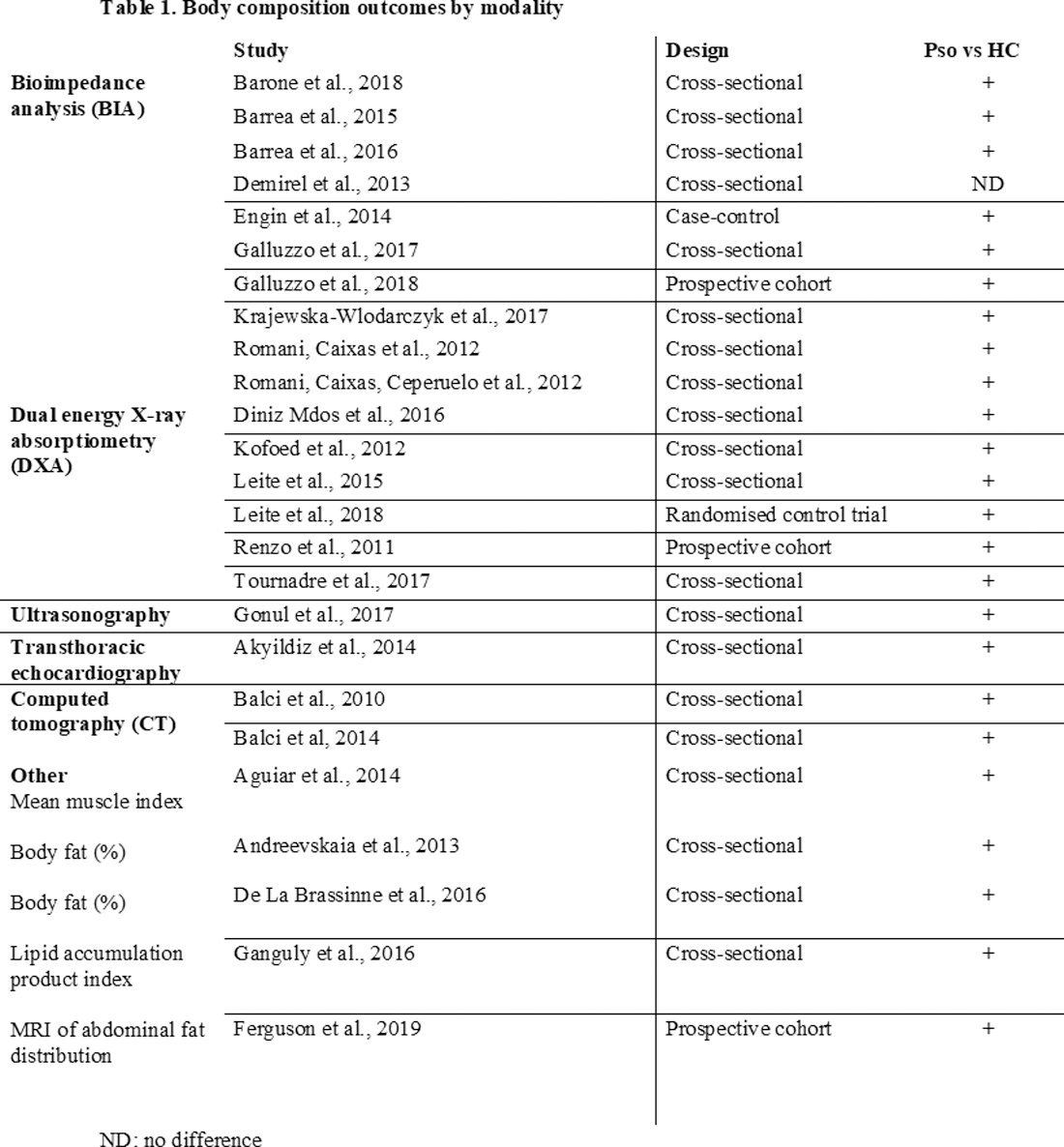
Results: Twenty-five whole-text papers met the inclusion criteria and were included in the final narrative analysis. The studies were of heterogeneous design and used a range of objective measures to assess body composition, including bioimpedance analysis (BIA), dual energy X-ray absorptiometry (DXA) and computed tomography (CT). Few studies met all the quality assessment criteria. 24 studies confirmed discrete biological and body composition changes in patients with psoriatic disease, which correlated positively with other indicators of metabolic syndrome, including waist circumference, waist-to-hip ratio, weight, BMI, plasma concentrations of LDL-cholesterol, leptin and apolipoprotein-B.
Conclusion: There is an increased prevalence of metabolic, anthropometric and internal body composition derangements in psoriatic patients compared with controls, and these changes seem to be independent of obesity and the customary metabolic syndrome, including higher overall body fat, visceral fat and sarcopenia. Our study highlights the applicability of several imaging techniques in the evaluation of body composition in psoriatic patients, including some novel automated systems, and future studies should focus on validation and standardization of assessment tools both in research and clinical practice.
REFERENCES:
[1]Balci, A., Balci, D. D., Yonden, Z., Korkmaz, I., Yenin, J. Z., Celik, E., Okumus, N. and Egilmez, E. (2010) ‘Increased amount of visceral fat in patients with psoriasis contributes to metabolic syndrome’, Dermatology, 220(1), pp. 32-37.
[2]Engin, B., Kutlubay, Z., Yardimci, G., Vehid, H. E., Ambarcioglu, P., Serdaroglu, S. and Tuzun, Y. (2014) ‘Evaluation of body composition parameters in patients with psoriasis’, International Journal of Dermatology, 53(12), pp. 1468-1473.
[3]Krajewska-Wlodarczyk, M., Owczarczyk-Saczonek, A. and Placek, W. (2017) ‘Changes in body composition and bone mineral density in postmenopausal women with psoriatic arthritis’, Reumatologia, 55(5).
[4]Welsh, P., Brown, R., Tindell, A., Kerrigan, S., Sattar, N., McInnes, I. and Siebert, S. ‘Effect of Phosphodiesterase 4 Inhibition with Apremilast on Cardiometabolic Outcomes in Psoriatic Arthritis – Initial Results from the Immune Metabolic Associations in Psoriatic Arthritis (IMAPA) Study’, Conference: ACR/ARP Annual Meeting , Atlanta.
Disclosure of Interests: None declared