Background: Conventional synthetic disease modifying anti-rheumatic drugs (csDMARDs) are the first-line treatment for psoriatic arthritis (PsA), but there is conflicting data regarding their efficacy and scarce reports describing the duration of use (drug retention) of csDMARD in this population. Their position in treatment recommendations is a matter of growing debate due the availability of alternative treatment options with higher levels of evidence.
Objectives: To study drug retention and predictors for drug retention among PsA patients receiving first-line csDMARD monotherapy.
Methods: Retrospective cohort study in DMARD-naïve adult PsA patients in whom a first csDMARD was prescribed as monotherapy primarily to treat PsA-related symptoms. Main outcome was time to failure of the csDMARD (i.e stopping the csDMARD or adding another DMARD).
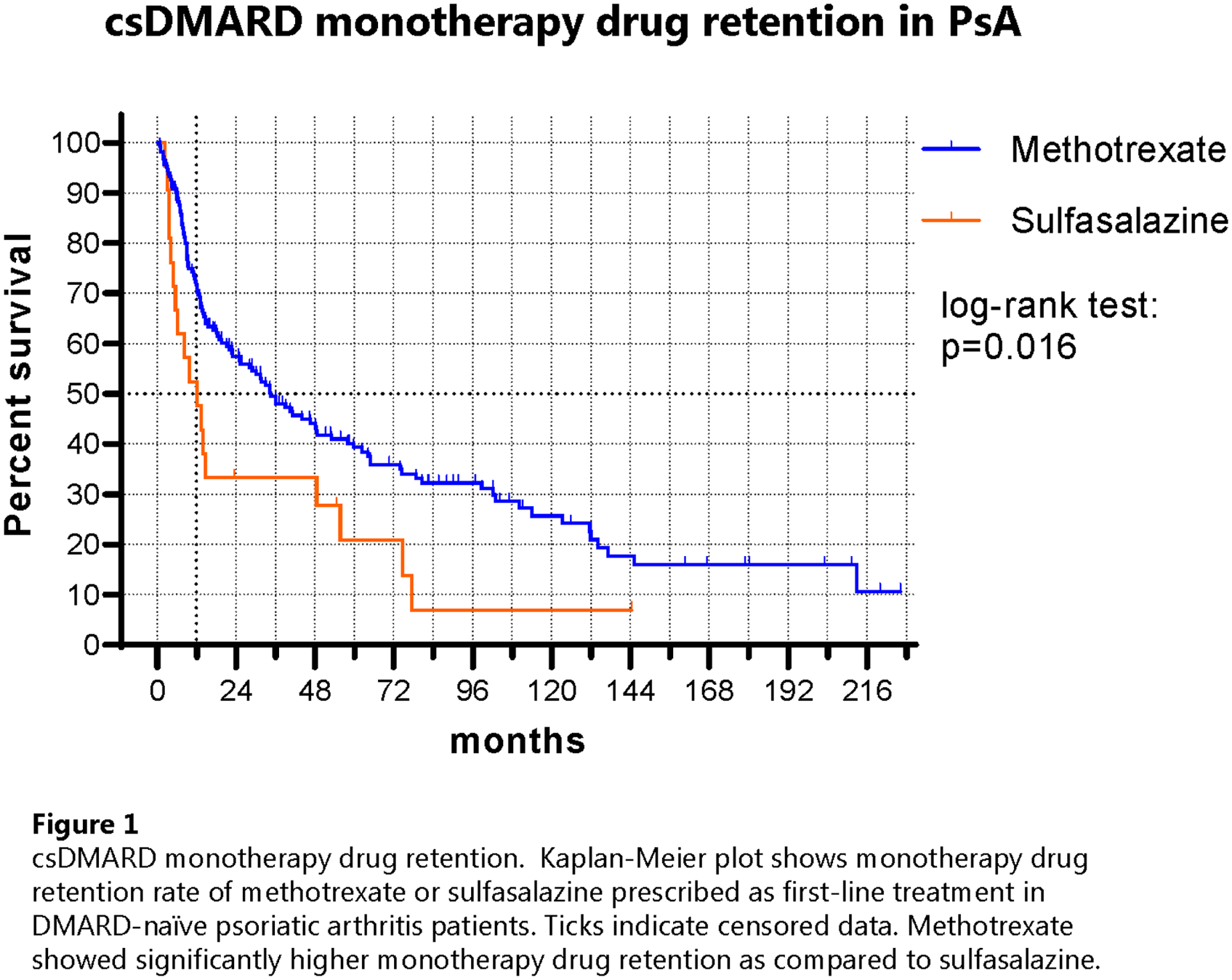
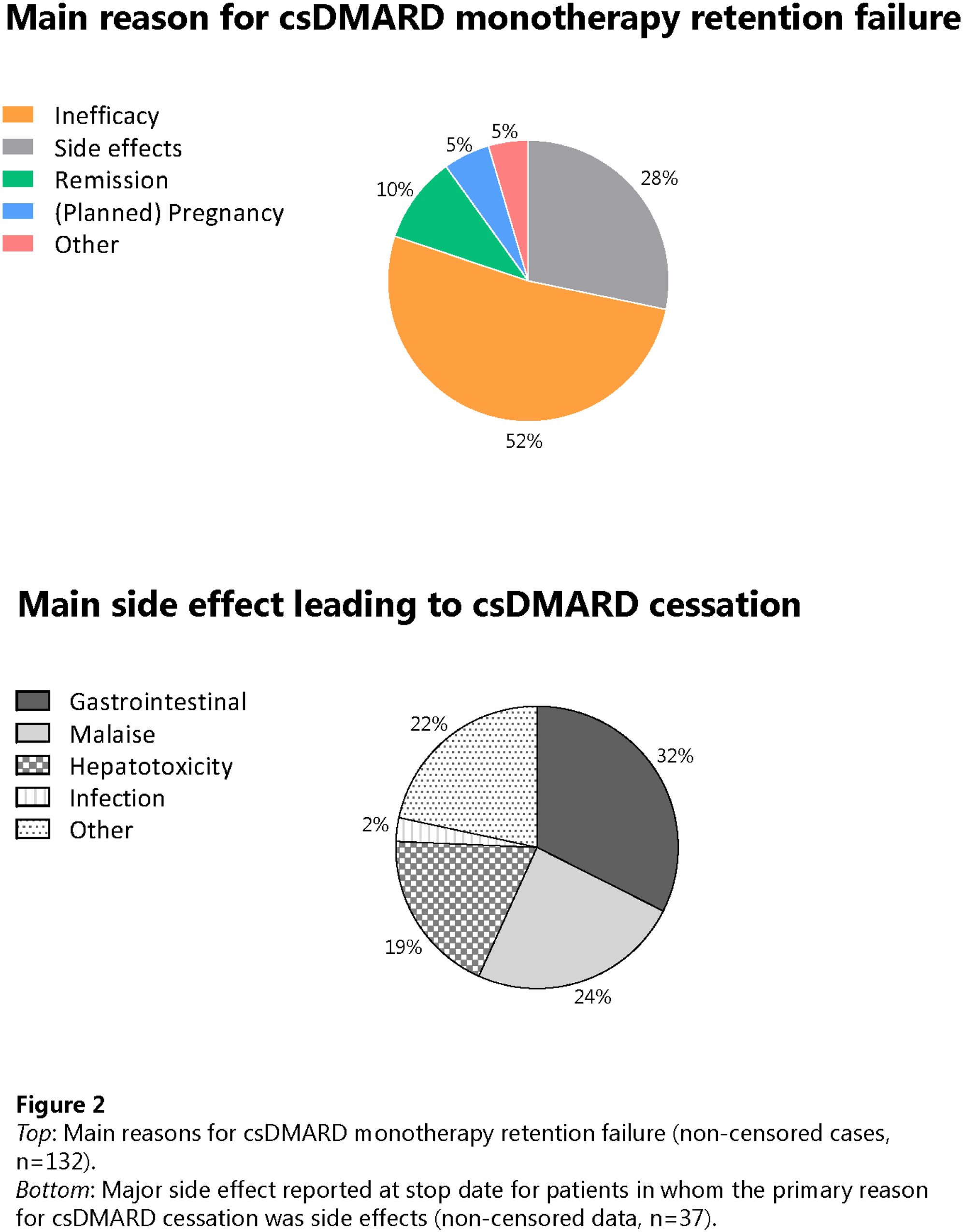
Results: 187 patients were included, who were mainly prescribed methotrexate (MTX) (n=163) or sulfasalazine (SSZ) (n=21) (
Main demographic and clinical characteristics of the study population at baseline. The total cohort (n=187) included 3 patients treated with leflunomide (data not shown separately). Psoriasis area and severity scores were unavailable for most cases and not shown. Descriptive data show the mean ± SD, median (IQR) or N (%).
| Total, N = 187 | MTX, N = 163 | SSZ, N = 21 | |
|---|---|---|---|
| Male, N (%) | 128 (31.6) | 115 (71) | 12 (57) |
| Age (years), mean ± SD* | 48.3 ± 13.3 | 49.1 ± 12.7 | 39.5 ± 13.4 |
| Body mass index, mean ± SD* | 26.7 ± 4.5 | 27.4 ± 4.4 | 25.3 ± 3.5 |
| Smoker, N (%) | 34/150 (18.2) | 31/129 (19.0) | 3/18 (14.3) |
| Disease duration (years), median (IQR) | |||
| PsA | 0.4 (0.1 – 3.0) | 0.4 (0.1 – 2.9) | 0.3 (0.1 – 2.0) |
| Psoriasis | 7.5 (2.1 – 18.4) | 7.5 (2.0 – 15.7) | 10.8 (3.1 – 26.7) |
| Psoriasis phenotype, N (%)* | |||
| Vulgaris only | 130/185 (69.5) | 117/161 (71.8) | 10/21 (47.6) |
| Sine psoriasis | 31/185 (16.6) | 21/161 (12.9) | 10/21 (47.6) |
| Other types 1 | 24/185 (12.8) | 23/161 (14.1) | 1/21 (4.8) |
| Nail disease present, N (%) | 81/121 (43.3) | 72/104 (44.2) | 9/17 (42.9) |
| Swollen joint count, median (IQR)* | 4 (2 – 6) | 4 (2 – 6) | 2 (1 – 3) |
| Tender joint count, median (IQR)* | 4 (1 – 6) | 4 (2 – 6) | 1 (0 – 3) |
| Dactylitis present, N (%) | 18/161 (9.6) | 17/142 (10.4) | 1/17 (4.8) |
| Axial disease present 2 , N (%) | 27/185 (14.4) | 24/161 (14.7) | 3/21 (14.3) |
| CRP, median (IQR) | 8.0 (2.9 – 16.0) | 8.0 (3.0 – 15.0) | 10.0 (1.0 – 26.0) |
| ESR, median (IQR) | 14.0 (6.0 – 27.5) | 14.0 (7.0 – 27.0) | 16.0 (6.0 – 31.0) |
| Erosive disease, N (%) | 40/156 (21.4) | 37/140 (22.7) | 2/15 (9.5) |
1 Other psoriasis types included guttate, palmoplantaris, inverse, and mixed types.
2 Presence/absence of axial disease was based on the clinical diagnosis from the treating physician.
* Clinical parameter is significantly different (P <0.05) between MTX and SSZ.
Abbreviations : MTX = methotrexate. SSZ = sulfasalazine. CRP = C-reactive protein. ESR = erythrocyte sedimentation rate. PsA = psoriatic arthritis.
Conclusion: MTX outperformed SSZ as first-line csDMARD monotherapy in DMARD-naïve PsA patients with respect to drug retention in daily clinical practice.
REFERENCES:
n.a.
Disclosure of Interests: Marleen Jacobs: None declared, Juliette Pouw: None declared, Paco Welsing: None declared, Timothy RDJ Radstake Employee of: TR currently is an employee of AbbVie. At the time of the work described he had no COIs., Emmerik Leijten: None declared