

Background: Posterior segment involvement is the most serious affection of uveitis in Behçet’s disease (BD), with cystoid macular edema (CME) being the leading cause of blindness. Anti-TNF, especially adalimumab (ADA) and infliximab (IFX), have demonstrated efficacy as first-line biologic agents in BD-related uveitis [1,2] . Moreover, the anti-IL6R tocilizumab (TCZ) has shown excellent results in highly refractory BD-uveitis and noninfectious uveitic CME [3-6] .
Objectives: To compare the efficacy of ADA vs IFX vs TCZ in patients with refractory CME due to BD.
Methods: Observational multicenter study of patients with BD-associated CME refractory to conventional and/or biological immunosuppressive drugs. From a cohort of 177 patients treated with anti-TNF and 14 patients treated with TCZ, we selected those with CME at baseline. CME was defined as macular thickness > 300μm (measured by optic coherence tomography). We analyzed in the 3 groups of treatment (ADA, IFX, TCZ) from baseline up to 4 years the evolution of macular thickness (main outcome) and best-corrected visual acuity (BCVA). Differences between basal and final follow-up were evaluated. Multivariable linear regression was used to assess the differences between the 3 groups.
Results: A total of 49 patients were included. ADA was used in 25 patients (40 eyes with CME), IFX in 15 (21 eyes with CME) and TCZ in 9 (11 eyes with CME). No statistically significant baseline differences were observed between the 3 groups (
Demographic and clinical characteristics of 49 patients with cystoid macular edema due to Behçet’s disease receiving ADA, IFX or TCZ.
| ADA (n=25 ) | IFX (n=15 ) | TCZ (n=9 ) | |
| Eyes with cystoid macular edema, n | 40 | 21 | 11 |
| Age, years | 41 ± 11 | 38 ± 9 | 43 ± 16 |
| Sex, men/women | 12/13 | 7/8 | 5/4 |
| HLA–B51 +, n | 19 | 10 | 6 |
| Duration of uveitis before anti-TNF/ anti-IL6R, months | 30 [12-82] | 15 [8-60] | 32 [24-144] |
| Ocular features at start of anti-TNF/anti-IL6R | |||
| Macular thickness, μm | 432 ± 118 | 483 ± 126 | 417 ± 113 |
| Visual acuity, BCVA | 0.4 ± 0.2 | 0.3 ± 0.2 | 0.2 ± 0.2 |
| Tyndall, inflammation grade | 2 [1-3] | 1 [0-1.5] | 1 [0-1.5] |
| Vitritis, inflammation grade | 2.5 [1.5-3] | 1 [0-2] | 2 [1-2] |
| Previous treatment, n | |||
| Oral glucocorticoids // i.v. pulse methylprednisolone | 18 // 13 | 4 // 9 | 7 // 8 |
| MTX //CsA //AZA | 13 // 22 // 14 | 8 // 13 // 8 | 8 // 6 // 2 |
| ADA // IFX | 0 // 0 | 0 // 0 | 7 // 3 |
| Prednisone dosage at start of anti-TNF/anti-IL6R, mg/day | 45 [30-60] | 30 [20-60] | 30 [30-30] |
| Combined treatment, n | |||
| CsA // AZA // MTX | 10 // 10 // 4 | 5 // 5 // 2 | 1 // 1 // 3 |
Data are presented as mean ± SD or median [IQR] when data were not normally distributed. ADA, adalimumab; AZA, azathioprine; CsA, cyclosporine A; MTX, methotrexate; IFX, infliximab; TCZ, tocilizumab.
Evolution of ocular parameters in 49 patients with cystoid macular edema due to Behçet’s disease receiving ADA, IFX or TCZ.
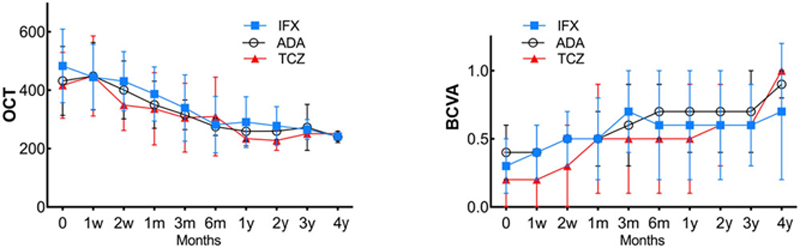
Conclusion: Refractory CME associated to BD’s uveitis can be effectively treated with ADA, IFX or TCZ. Moreover, TCZ is effective in patients resistant to anti-TNF therapy.
REFERENCES:
[1] Arthritis Rheumatol. 2019;71(12):2081-2089. doi: 10.1002/art.41026
[2] Ophthalmology. 2018;125(9):1444-1451. doi: 10.1016/j.ophtha.2018.02.020
[3] Rheumatology (Oxford). 2018;57(5):856-864. doi: 10.1093/rheumatology/kex480
[4] Am J Ophthalmol. 2019;200:85-94. doi: 10.1016/j.ajo.2018.12.019
[5] Clin Exp Rheumatol. 2014;32(4 Suppl 84): S54-7. PMID: 25005576
[6] Clin Exp Rheumatol. 2016;34(6 Suppl 102): S34-S40. PMID:27054359
Disclosure of Interests: None declared