

Background: Acute Respiratory Distress Syndrome (ARDS) is a life-threatening complication of COVID-19 and has been reported in approximately one-third of hospitalized patients with COVID-19 1 . Risk factors associated with the development of ARDS include older age and diabetes 2 . However, little is known about factors associated with ARDS in the setting of COVID-19, in patients with rheumatic disease or those receiving immunosuppressive medications. Prediction algorithms using traditional regression methods perform poorly with rare outcomes, often yielding high specificity but very low sensitivity. Machine learning algorithms optimized for rare events are an alternative approach with potentially improved sensitivity for rare events, such as ARDS in COVID-19 among patients with rheumatic disease.
Objectives: We aimed to develop a prediction model for ARDS in people with COVID-19 and pre-existing rheumatic disease using a series of machine learning algorithms and to identify risk factors associated with ARDS in this population.
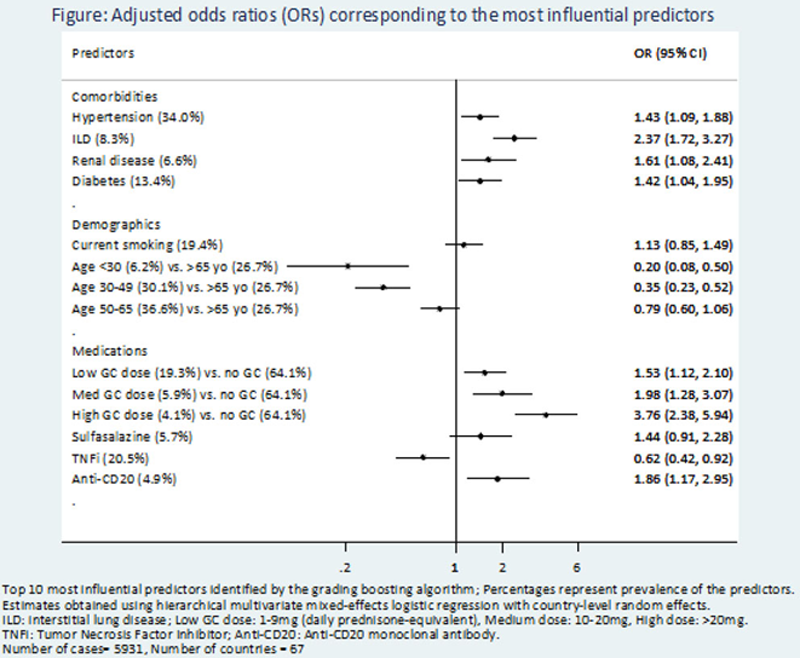
Methods: We used data from the COVID-19 Global Rheumatology Alliance (GRA) Registry from March 24 to Nov 1, 2020. ARDS diagnosis was indicated by the reporting clinician. Five machine learning algorithms optimized for rare events predicted ARDS using 42 variables covering patient demographics, rheumatic disease diagnoses, medications used at the time of COVID-19 diagnosis, and comorbidities. Model performance was assessed using accuracy, area under curve, sensitivity, specificity, positive predictive value, and negative predictive value. Adjusted odds ratios corresponding to the 10 most influential predictors from the best performing model were derived using hierarchical multivariate mixed-effects logistic regression that accounted for within-country correlations.
Results: A total of 5,931 COVID-19 cases from 67 countries were included in the analysis. Mean (SD) age was 54.9 (16.0) years, 4,152 (70.0%) were female, and 2,399 (40.5%) were hospitalized. ARDS was reported in 388 (6.5% of total and 15.6% of hospitalized) cases. Statistically significant differences in the risk of ARDS were observed by demographics, diagnoses, medications, and comorbidities using unadjusted univariate comparisons (data not shown). Gradient boosting machine (GBM) had the highest sensitivity (0.81) and was considered the best performing model (
Performance of machine learning algorithms.
| GBM | SVM | GLMNET | NNET | RF | |
| Accuracy | 0.79 | 0.68 | 0.66 | 0.66 | 0.67 |
| AUC | 0.75 | 0.70 | 0.74 | 0.58 | 0.74 |
| Sensitivity | 0.81 | 0.68 | 0.65 | 0.68 | 0.67 |
| Specificity | 0.49 | 0.60 | 0.73 | 0.48 | 0.68 |
| PPV | 0.96 | 0.96 | 0.97 | 0.95 | 0.97 |
| NPV | 0.16 | 0.12 | 0.13 | 0.09 | 0.13 |
GBM: Gradient Boosting Machine, SVM: Support vector machines, GLMNET: Lasso and Elastic-Net Regularized Generalized Linear Models, NNET: Neural Networks, RF: Random Forest. AUC: Area Under Curve; PPV: Positive Predictive Value; NPV: Negative Predictive Value.
Conclusion: In this global cohort of patients with rheumatic disease, a machine learning model, GBM, predicted the onset of ARDS with 81% sensitivity using baseline information obtained at the time of COVID-19 diagnosis. These results identify patients who may be at higher risk of severe COVID-19 outcomes. Further studies are necessary to validate the proposed prediction model in external cohorts and to evaluate its clinical utility. Disclaimer: The views expressed here are those of the authors and participating members of the COVID-19 Global Rheumatology Alliance, and do not necessarily represent the views of the ACR, NIH, (UK) NHS, NIHR, or the department of Health.
REFERENCES:
[1]Tzotzos SJ, Fischer B, Fischer H, Zeitlinger M. 2020;24(1):516.
[2]Wu C, Chen X, Cai Y, et al. JAMA Intern Med. 2020;180(7):934-943.
Acknowledgements: The COVID-19 Global Rheumatology Alliance.
Disclosure of Interests: Zara Izadi: None declared, Milena Gianfrancesco: None declared, Kimme Hyrich Speakers bureau: Abbvie and grant income from BMS, UCB, and Pfizer, all unrelated to this study., Anja Strangfeld Speakers bureau: AbbVie, MSD, Roche, BMS, Pfizer, outside the submitted work., Grant/research support from: A consortium of 13 companies (among them AbbVie, BMS, Celltrion, Fresenius Kabi, Lilly, Mylan, Hexal, MSD, Pfizer, Roche, Samsung, Sanofi-Aventis, and UCB) supporting the German RABBIT register., Laure Gossec Consultant of: Abbvie, Biogen, Celgene, Janssen, Lilly, Novartis, Pfizer, Sanofi-Aventis, UCB., Grant/research support from: Lilly, Mylan, Pfizer, all unrelated to this study., Loreto Carmona Consultant of: Loreto Carmona’s institute works by contract for laboratories among other institutions, such as Abbvie Spain, Eisai, Gebro Pharma, Merck Sharp & Dohme España, S.A., Novartis, Farmaceutica, Pfizer, Roche Farma, Sanofi Aventis, Astellas Pharma, Actelion Pharmaceuticals España, Grünenthal GmbH, and UCB Pharma., Elsa Mateus Grant/research support from: LPCDR received grants from Abbvie, Novartis, Janssen-Cilag, Lilly Portugal, Sanofi, Grünenthal S.A., MSD, Celgene, Medac, Pharmakern, GAfPA and Pfizer., Saskia Lawson-Tovey: None declared, Laura Trupin: None declared, Stephanie Rush: None declared, Gabriela Schmajuk: None declared, Lindsay Jacobsohn: None declared, Patti Katz: None declared, Samar Al Emadi: None declared, Leanna Wise: None declared, Emily Gilbert: None declared, Maria Valenzuela-Almada: None declared, Ali Duarte-Garcia: None declared, Jeffrey Sparks Consultant of: Bristol-Myers Squibb, Gilead, Inova, Janssen, and Optum unrelated to this work., Grant/research support from: Amgen and Bristol-Myers Squibb., Tiffany Hsu: None declared, Kristin D’Silva: None declared, Naomi Serling-Boyd: None declared, Suleman Bhana Employee of: Suleman Bhana reports non-branded marketing campaigns for Novartis (<$10,000)., Wendy Costello: None declared, Rebecca Grainger Speakers bureau: Abbvie, Janssen, Novartis, Pfizer, Cornerstones and travel assistance from Pfizer (all < $10,000)., Jonathan Hausmann Consultant of: Novartis, unrelated to this work (<$10,000)., Jean Liew Grant/research support from: Pfizer, outside the submitted work., Emily Sirotich Grant/research support from: Emily Sirotich is a Board Member of the Canadian Arthritis Patient Alliance, a patient run, volunteer-based organization whose activities are largely supported by independent grants from pharmaceutical companies., Paul Sufka: None declared, Zachary Wallace Consultant of: Viela Bio and MedPace, outside the submitted work., Grant/research support from: Bristol-Myers Squibb and Principia/Sanofi., Pedro Machado Speakers bureau: Abbvie, BMS, Celgene, Eli Lilly, Janssen, MSD, Novartis, Pfizer, Roche and UCB, all unrelated to this study (all < $10,000)., Philip Robinson Consultant of: Abbvie, Eli Lilly, Janssen, Novartis, Pfizer and UCB and travel assistance from Roche (all < $10,000)., Jinoos Yazdany Consultant of: Eli Lilly and Astra Zeneca, unrelated to this project.