

Background: Upadacitinib (UPA), an oral Janus kinase inhibitor, demonstrated significant improvements in signs, symptoms, and structural inhibition as monotherapy (mono) vs methotrexate (MTX) in MTX-naïve patients (pts) with rheumatoid arthritis (RA) through 48 weeks (wks). 1
Objectives: To report the efficacy and safety of UPA vs MTX mono up to 156 wks in pts with RA from the ongoing long-term extension (LTE) of the SELECT-EARLY trial.
Methods: During the 48-wk double-blind study period, pts were randomized to UPA 15 or 30 mg once daily (QD) or MTX (titrated to 20 mg/wk by Wk 8). At Wk 26, pts who did not achieve Clinical Disease Activity Index (CDAI) remission (≤2.8) and had <20% improvement from baseline in tender or swollen joint count received blinded rescue therapy (addition of MTX for UPA groups and UPA 15 or 30 mg for MTX group). In the LTE, pts received open-label treatment once the last pt reached Wk 48. Efficacy assessments up to Wk 156 were summarized by randomized group and included American College of Rheumatology (ACR) responses, remission and low disease activity (LDA) measures, and change in modified Total Sharp Score (mTSS; up to 96 wks). Treatment-emergent adverse events (AEs) per 100 pt-years (PY) for pts on continuous mono were summarized through 156 wks. Non-responder imputation was used for binary endpoints for missing data and when pts received rescue therapy or prematurely discontinued the study drug.
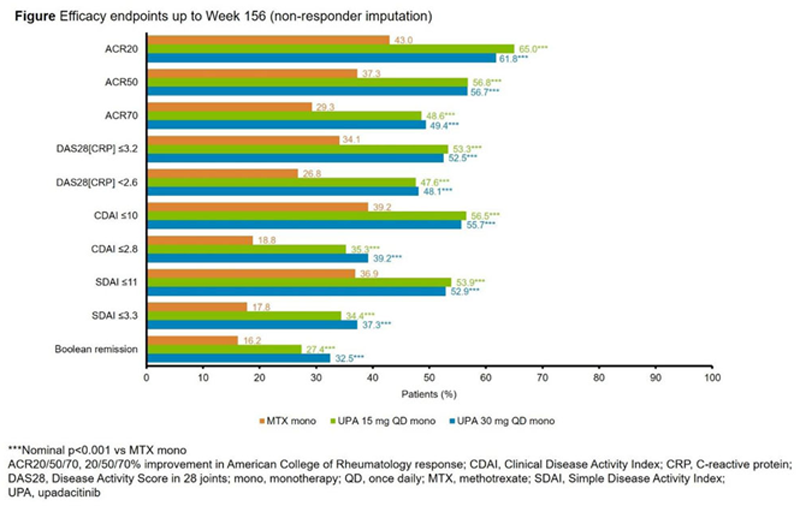
Results: Of 945 pts randomized and treated, 775 entered the LTE on study drug (including 57 rescued pts; MTX, 33; UPA 15 mg, 17; UPA 30 mg, 7). Overall, 161 (21%) pts discontinued during the LTE. At Wk 156, higher proportions of pts randomized to UPA achieved a 20/50/70% improvement in ACR response (ACR20/50/70), LDA, and remission vs MTX (
Conclusion: UPA monotherapy showed sustained clinically meaningful responses including remission vs MTX through Wk 156 but higher rates of several AEs, including HZ, neutropenia, and CPK elevations; no new safety risks were observed compared with previous results. 1,2
REFERENCES:
[1]van Vollenhoven R, et al. Ann Rheum Dis 2019;78:376–7; 2. Cohen SB, et al. Ann Rheum Dis 2020;annrheumdis-2020-218510.
Safety overview
| E/100 PY (95% CI) | MTX mono
| UPA 15 mg QD mono
| UPA 30 mg QD mono
|
| Any AE | 240.2
| 268.0
| 292.5
|
| Any serious AE | 10.8 (8.3, 13.8) | 12.2 (9.8, 15.1) | 16.3 (13.4, 19.6) |
| Any AE leading to discontinuation of study drug | 6.5 (4.6, 8.9) | 7.3 (5.4, 9.5) | 7.7 (5.8, 10.1) |
| Any death a | 0.7 (0.2, 1.7) | 0.9 (0.3, 1.9) | 1.0 (0.4, 2.1) |
| Serious infection | 2.5 (1.4, 4.1) | 3.3 (2.1, 4.9) | 4.4 (2.9, 6.2) |
| Opportunistic infection excluding TB and HZ | 0.2 (0.0, 0.9) | 0.1 (0.0, 0.8) | 0.3 (0.0, 1.1) |
| HZ | 0.8 (0.3, 1.9) | 4.5 (3.1, 6.4) | 4.7 (3.2, 6.6) |
| Active TB | 0 | 0.3 (0.0, 1.0) | 0.3 (0.0, 1.1) |
| NMSC | 0 | 0.4 (0.1, 1.2) | 1.0 (0.4, 2.1) |
| Malignancy other than NMSC | 1.0 (0.4, 2.2) | 0.6 (0.2, 1.5) | 1.2 (0.5, 2.3) |
| Hepatic disorder | 14.1 (11.3, 17.5) | 12.5 (10.0, 15.4) | 15.0 (12.2, 18.2) |
| GI perforation b | 0 | 0 | 0.4 (0.1, 1.3) |
| Neutropenia | 2.2 (1.2, 3.7) | 4.5 (3.1, 6.4) | 5.7 (4.0, 7.8) |
| CPK elevation | 1.8 (0.9, 3.3) | 7.7 (5.8, 10.0) | 15.4 (12.6, 18.6) |
| MACE b | 0.3 (0.0, 1.2) | 0.4 (0.1, 1.2) | 0.6 (0.2, 1.5) |
| VTE b | 0.3 (0.0, 1.2) | 0.4 (0.1, 1.2) | 0.6 (0.2, 1.5) |
Data were censored at the time of MTX or UPA addition for rescued pts
a Includes treatment-emergent (≤30 days after the last dose of study drug) and non-treatment-emergent deaths. b Adjudicated
Acknowledgements: AbbVie funded this study; contributed to its design; participated in data collection, analysis, and interpretation of the data; and in the writing, review, and approval of the abstract. No honoraria or payments were made for authorship. Medical writing support was provided by Russell Craddock, PhD, of 2 the Nth (Cheshire, UK), and was funded by AbbVie.
Disclosure of Interests: Ronald van Vollenhoven Speakers bureau: AbbVie, AstraZeneca, Biotest, Bristol-Myers Squibb, Galapagos, Gilead, GSK, Janssen, Pfizer, Sanofi, Servier, UCB, and Viela Bio, Consultant of: AbbVie, AstraZeneca, Biogen, Biotest, Bristol-Myers Squibb, Galapagos, Gilead, GSK, Janssen, Pfizer, Sanofi, Servier, UCB, and Viela Bio, Grant/research support from: Bristol-Myers Squibb, GSK, Eli Lilly, Pfizer, Roche, and UCB, Tsutomu Takeuchi Speakers bureau: AbbVie, AYUMI, Bristol-Myers Squibb, Chugai, Daiichi Sankyo, Dainippon Sumitomo, Eisai, Gilead, Mitsubishi Tanabe, Novartis, Pfizer, and Sanofi, Consultant of: Astellas, Chugai, and Eli Lilly, Grant/research support from: AbbVie, Asahi Kasei, Astellas, Chugai, Daiichi Sankyo, Eisai, Mitsubishi Tanabe, Nippon Kayaku, Shionogi, Takeda, and UCB, Jacob Aelion Grant/research support from: AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Celgene, Eli Lilly, Galapagos/Gilead, Genentech, GSK, Horizon, Janssen, Mallinckrodt, Nektar, Nichi-Iko, Novartis, Pfizer, Regeneron, Roche, Sanofi, Selecta, and UCB, Nilmo Chávez Speakers bureau: AbbVie, Janssen, and Pfizer, Consultant of: AbbVie, Janssen, and Pfizer, Grant/research support from: AbbVie, Galapagos, Gilead, Pfizer, and Sanofi, Pablo Mannucci Walter Consultant of: AbbVie, Grant/research support from: AbbVie, Bristol-Myers Squibb, Eli Lilly, Genentech/Roche, GSK, Janssen, and UCB, Atul Singhal Consultant of: AbbVie, Aclaris, Amgen, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Gilead, Idorsia, Novartis, Oscotec, Pfizer, Regeneron, Roche/Genentech, Sanofi, Selecta, Takeda, UCB, and Viela Bio, Grant/research support from: AbbVie, Aclaris, Amgen, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Gilead, Idorsia, Novartis, Oscotec, Pfizer, Regeneron, Roche/Genentech, Sanofi, Selecta, Takeda, UCB, and Viela Bio, Jerzy Swierkot Speakers bureau: AbbVie, Accord, BMS, Janssen, MSD, Pfizer, Roche, Sandoz, and UCB, Consultant of: AbbVie, Accord, BMS, Janssen, MSD, Pfizer, Roche, Sandoz, and UCB, Grant/research support from: AbbVie, Accord, BMS, Janssen, MSD, Pfizer, Roche, Sandoz, and UCB, Alan Friedman Shareholder of: May own stock or options in AbbVie, Employee of: AbbVie, Nasser Khan Shareholder of: May own stocks or options in AbbVie, Employee of: AbbVie, Yihan Li Shareholder of: May own stocks or options in AbbVie, Employee of: AbbVie, Xianwei Bu Shareholder of: May own stocks or options in AbbVie, Employee of: AbbVie, Justin Klaff Shareholder of: May own stock or options in AbbVie, Employee of: AbbVie, Vibeke Strand Consultant of: AbbVie, Amgen, Arena, AstraZeneca, Bayer, Bristol-Myers Squibb, Boehringer Ingelheim, Celltrion, Eli Lilly, Genentech/Roche, Gilead, GSK, Ichnos, Inmedix, Janssen, Kiniksa, MSD, Myriad Genetics, Novartis, Pfizer, Regeneron, Sandoz, Sanofi, Setpoint, and UCB