

Background: Rhupus is a term that describe the coexistence of systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). Rhupus patients have symmetrical, erosive arthritis, characteristic SLE manifestations and an array of autoantibodies including rheumatoid factor (RF), anti-cyclic citrullinated peptides (anti-CCP), anti-dsDNA, and anti-Sm. 1 Joint involvement is common in SLE patients (90%), but only 1% to 9,7% have rhupus. 2 Due to its low prevalence, there is still a lack of evidence on its presentation and differences with other SLE patients without rhupus.
Objectives: To examine the rhupus prevalence and to compare the clinical and serological characteristics between rhupus, and non-rhupus SLE patients (SLE with arthritis (SLEa), and SLE without arthritis (SLEwa)).
Methods: We performed a case-control study. Rhupus patients (cases) were matched 1:1 with non-rhupus SLE patients (controls). Descriptive statistics were calculated and rhupus, SLEa, and SLEwa were compared.
Results: A total of 72 patients were included, 24 patients in each group; most were female (87.5%). The median age at rhupus onset was 36.5 years (IQR 30-42.5). RA preceded rhupus in half of the patients, 29% were initially diagnosed as SLE, and 21% were initially diagnosed as rhupus. The median duration of RA was 66 months (IQR 30-144).
In the descriptive analysis of rhupus patients, the most affected joints were the proximal interphalangeal and metacarpophalangeal joints (87.5%), followed by the wrists (79.1%). Regarding immunological findings, RF and anti-CCP were positive in 87.5% and 50% of the patients, respectively. As to radiographic findings, the median number of erosions in the hands and wrists was 2 (IQR 0-5) and the median number of joints with narrowed joint space was 7 (IQR: 1.5 - 13.5). In terms of treatment, 95.8% received corticosteroids (median 10 mg/day), 91.6% antimalarials, 79.1% methotrexate, 41.6% leflunomide, and 25.0% rituximab.
Patients with rhupus were older and had less renal and hematological involvement than patients with SLEa and SLEwa. SLEa patients had higher seropositivity for anti-RNP and anti-Sm, higher neurological involvement, and higher SLEDAI-2K scores than rhupus patients. Comparisons of other clinical and serological variables between SLE rhupus and non-ruphus patients are shown in
Clinical and serological manifestations in rhupus, articular SLE, and non-articular SLE
| Variables |
RHUPUS
|
SLE with arthritis
|
SLE without arthritis
| P value RHUPUS vs. SLE with arthritis |
p value RHUPUS
|
| Age (years) M (IQR) | 40 (31.5 – 49) | 29 (21.5 – 45) | 33 (19.5 – 37.5) | 0.043 | 0.013 |
| CPR M (IQR) | 2.3 (1– 8.5) | 1.6 (0.3– 3.6) | 0.9 (0.2– 2.5) | 0.337 | 0.032 |
| Positive anti-RNP N (%) | 7 (29.1%) | 14 (58.3%) | 7 (29.1%) | 0.042 | 1.000 |
| Positive anti-Sm N (%) | 5 (20.8%) | 15 (62.5%) | 6 (25%) | 0.003 | 0.500 |
| SLEDAI – 2K score M (IQR) | 4.5 (1 – 7) | 9 (2 – 18) | 7 (3.5 – 15) | 0.045 | 0.082 |
Differences in the frequencies of organic alterations. w/o: without.
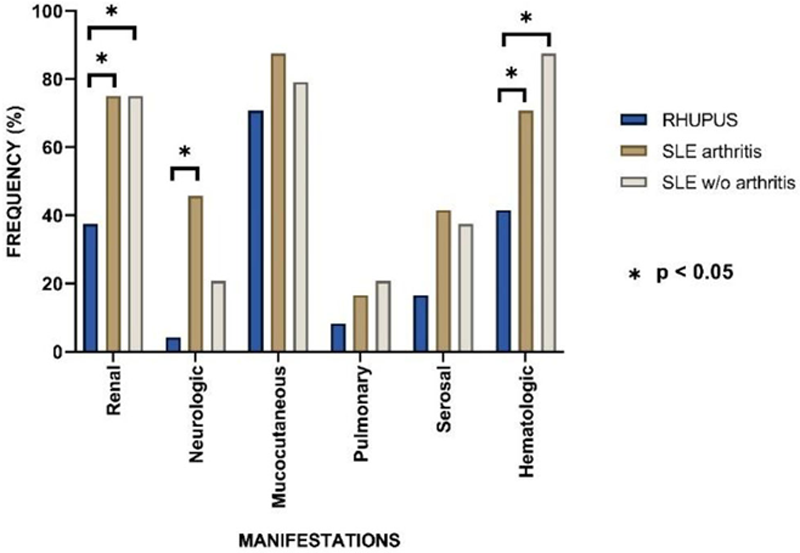
Conclusion: Patients with rhupus were older and had lower SLEDAI-2K scores compared with those non-rhupus. Furthermore, renal, neurological, and hematological manifestations were more common in non-rhupus patients than in rhupus patients.
REFERENCES:
[1]Antonini L, et al. Rhupus: a systematic literature review. Autoimmun Rev. 2020;19(9):102612.
[2]Tani C, et al. Rhupus syndrome: Assessment of its prevalence and its clinical and instrumental characteristics in a prospective cohort of 103 SLE patients. Autoimmun Rev. 2013; 12:537–41.
Disclosure of Interests: None declared