

Background: Systemic sclerosis (SSc) may present distinctive manifestations and survival in different ethnic and geographic groups.
Objectives: To describe the clinical features, treatments, and survival of adult SSc patients registered in Reuma.pt/SSc.
Methods: Demographic features, SSc subsets, fulfilment of classification criteria, clinical and immunologic characteristics, comorbidities, medication and deaths were reviewed. Survival was calculated for patients included in the registry within the first 2 years of diagnosis.
Results: In total, 1054 patients were included, 87.5% female, mean age at diagnosis 52.7 ± 14.8 years. The most common subset was limited cutaneous (lc)SSc (56.3%), followed by diffuse cutaneous (dc)SSc (17.5%), preclinical SSc (13%), overlap syndrome (9.8%) and SSc sine scleroderma (3.3%). Raynaud’s phenomenon (93.4%) and skin thickening (76.9%) were the most observed manifestations. Gastrointestinal (62.8%
vs
47.8%), pulmonary (59.5%
vs
23%) and cardiac (12.8%
vs
6.9%) involvement were significantly more prevalent in dcSSc compared to lcSSc (
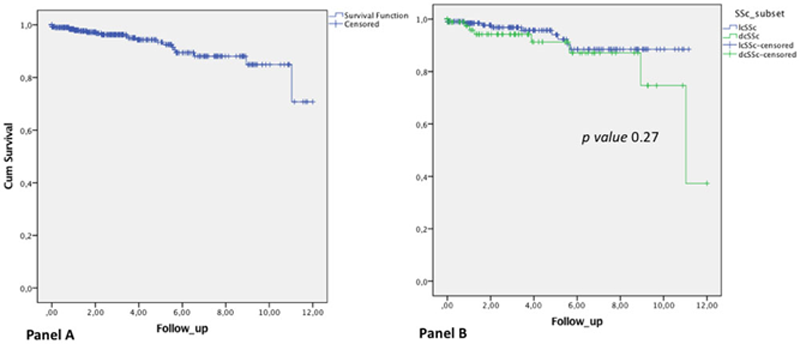
During the median follow-up 12.4 years, 83 deaths (7.9%) were verified. The overall 1, 2 and 5 years survival was 98.0%, 96.8% and 92.6% respectively, without significant differences between lcSSc and dcSSc (
Conclusion: Reuma.pt/SSc register is useful in routine patient monitoring and contributes to improve knowledge about this rare and complex disease. Clinical features of Portuguese SSc patients are similar to what has been described in other populations although the overall 5-year survival in recently diagnosed patients appears to be higher than previously reported.
Cumulative clinical and immunologic characteristics of Portuguese SSc patients
| Clinical and immunologic features |
Total
|
Limited cutaneous SSc
|
Diffuse cutaneous SSc
| P value |
| Skin involvement – N(%) N=987 | 688 (90.6) | 525 (90.7) | 180 (100) | <0.01 |
| Skin thickening * – N (%) N= 962 | 680 (76.9) | 512 (88.9) | 180 (100) | <0.01 |
| Digital ulcers – N (%) N=970 | 325(33.5) | 186 (34.7) | 4 (51.5) | <0.01 |
| Raynaud’s Phenomenon – N (%) N=1010 | 943 (93.4) | 539 (95.7) | 157 (92.4) | 0.06 |
| Musculoskeletal involvement – N(%) N=972 | 346 (45.6) | 247 (42.7) | 99 (55) | <0.01 |
| Cardiac involvement –N(%) – N=924 | 71 (7.7) | 36 (6.9) | 19 (12.8) | 0.02 |
| Renal involvement –N(%) – N= 917 | 17 (1.9) | 8!1.5) | 6 (4.1) | 0.07 |
| Gastrointestinal involvement - N(%) N=933 | 508 (48.2) | 277 (47.8) | 113 (62.8) | <0.01 |
| Pulmonary involvement – N(%) N=915 | 261 (28.5) | 119 (23) | 88 (59.5) | <0.01 |
| PAH – N(%) N= 871 | 14 (1.6) | 10 (2) | 1 (0.7) | 0.23 |
| Intersticial lung disease – N(%) N=765 | 218 (28.5) | 100 (22.7) | 75 (57.7) | <0.01 |
| Antinuclear antibodies - N(%) N=1040 | 934 (89.8) | 522 (90.2) | 154 (88.5) | 0.57 |
| Anti-centromere – N(%) N= 1027 | 540 (52.6) | 383 (67.1) | 16 (9.5) | <0.01 |
| Anti-Scl70 – N(%) N=1020 | 214 (21) | 12 (3.3) | 104 (60.1) | <0.01 |
| Anti-RNA polymerase III – N(%) N=710 | 25 (3.5) | 12 (3.3) | 7 (5.6) | 0.38 |
| Comorbidities | ||||
| Hypertension – N(%) N=431 | 117 (27.1) | 76 (29.7) | 67 (20.7) | 0.1 |
| Hyperlipidemia – N(%) N=431 | 71 (13.4) | 72 (12.2) | 24 (15.9) | 0.08 |
| Neoplasia – N(%) N=1054 | 29 (2.8) | 12 (2.1) | 7 (3.9) | 0.14 |
PDE-5 (phosdiasterase-5); PPIs (proton pump inhibitors); PAH-Pulmonary arterial hypertension confirmed by right heart catheterization. Immunomodulators includes Metothrexate, Leflunomide, Hydroxycloroquine; Azathioprine, Mycophenolate Mofetil and Cyclophosphamide; * Does not include sclerodactyly.
Panel A - Survival in years from diagnosis of patients with SSc included in Reuma.pt in the first 2 years of disease (N=472). Panel B - survival according to SSc subset (lcSSc and dcSSC).
Disclosure of Interests: None declared