

Background: Parenteral anti-osteoporotic medications are frequently recommended for the management of primary and secondary osteoporosis by NICE (1) and EULAR (2) guidelines.
Objectives: This audit aimed at evaluating the efficacy, adherence and safety profile of denosumab (D), zoledronate (Z) and teriparatide (T).
Methods: The data of patients initiating D, Z and T from 2012-2021 were retrospectively reviewed using electronic medical records at Basildon hospital.
Results: We enrolled 146 patients diagnosed with low bone density and on following treatment (3-6 years D (n: 50), 4-5 years Z (n: 50) and 2 years T (n: 46). More than 92% were Caucasian females; 41.7% were above 80 years.
T group had more pronounced reduction in bone mineral density (BMD) with a mean T-score
(spine:-3.9, hip: -2.6, neck of femur: -2.7; followed by Z group (spine: -2.6, hip:-2, neck of femur: -2.5) and D group (spine: -2.3, hip:-2.2, neck of femur: -2.3).
Primary prevention was in 26% and secondary prevention in 73.9%; with the commonest fractures at the vertebrae at 40%.
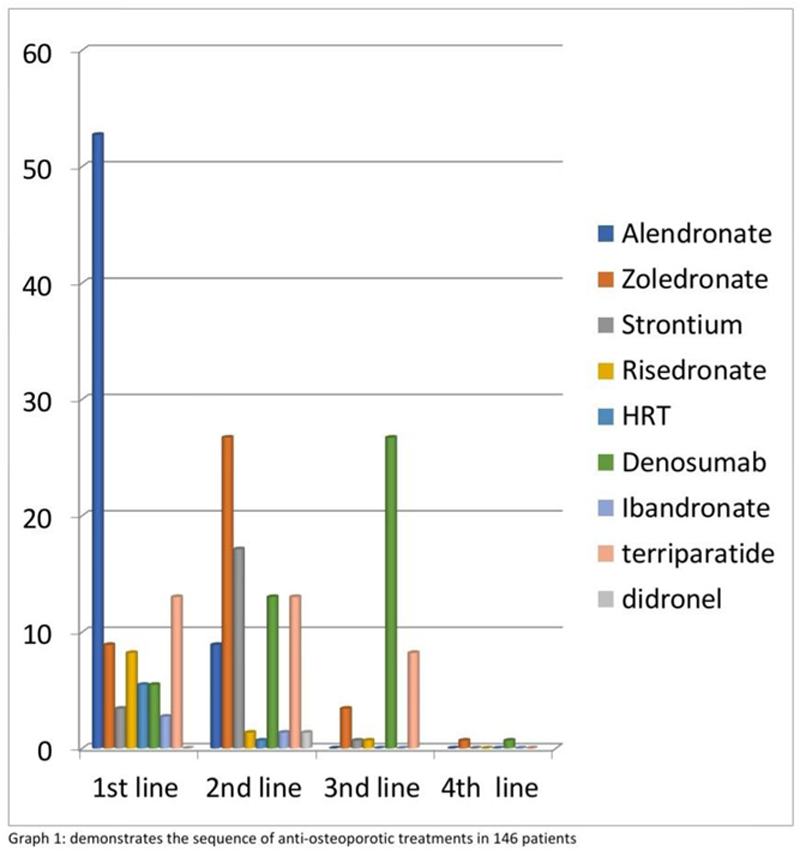
Oral bisphosphonate was the first choice in 63.6% of the cases (please see graph1). Intolerance, gastric upset or inefficacies were the commonest reasons to avoid them.
After the 3rd Z or 5th D, DXA scan shows improvements or stability in BMD at both hip and spinal areas in 88% and 82% respectively; compared to 69.6% after completing 2 years of T. The rate of improvement or stability plummeted after the 10th D and 5th Z (Please see
Monitoring BMD after courses of D, Z and T.
| DXA scan:
|
After
|
After
|
After
|
After
|
After
|
| Percentage of scanned patients | 100% | 90% | 100% | 60% | 71.73% |
| Improved or stable BMD at spine or hip areas | 82% | 75.5% | 88% | 85.6% | 69.6% |
| Improved or stable BMD at the spine but declined at hip area | 18% | 19.9% | 12% | 13.3% | 24.2% |
| Declined BMD at both spine and hip areas | 4.4% | 6% |
The course of T was stopped earlier in 28.2% of the cases due to the difficulty in taking injections or side effects including nausea, gastric upset, myalgia, insomnia, poor renal function, raised PTH, ALP and calcium. Dental issues (not osteonecrosis) were the reason to stop Z and D in 2% of each group and 8% choose to discontinue D after developing other non-related comorbidities. There were no fragility fractures during the treatment courses.
The outcome after reviewing 91.3% of those who completed or stopped the T course shows 39% commenced on D whereas 35.7% and 19% on Z and alendronate respectively leaving 7.1% on drug holiday. After completion of the 10th D, 78.5% of the reviewed patients were continued on further D injections whereas 3.5% were switched to T and 17.8% given drug holiday. For those who were reviewed after the 5th Z, 94% were switched to D and 5.8% given drug holiday.
Conclusion: D, Z and T were well tolerated and could effectively either maintain or improve the BMD at both spinal and hip sites and prevent fragility fractures and T was associated with the most pronounced soar in BMD. There were few cases of deterioration mainly at the hip area with all groups.
Prior bisphosphonate therapy did not show significant influence on the later effects of D, Z or T on BMD. After completion of the treatment for the 3 groups, only 30.87 % of the reviewed cases were advised for drug holiday and majority were switched to D as Z and T is limited to 5 and 2 years course respectively.
Heterogeneity in decision making exists due to variability in recommending these medications, patient preference and mode of administration. To optimize the adherence and effects of anti-osteoporotic medications, stratified guidelines is required for the long term use of these medications and discontinuation of D.
REFERENCES:
[1]NICE Pathway: 20 August 2019,
[2]Kanis JA et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019 Jan;30(1):3-44.
Disclosure of Interests: None declared.