

Background: Hip osteoarthritis (HOA) is a severe outcome of juvenile idiopathic arthritis (JIA) itself and also can be result of corticosteroid (CS) treatment, if it was used. Total hip arthroplasty (THA) is the last step in JIA treatment and indicates ineffectiveness of conservative treatment.
Objectives: We aimed to evaluate risk factors which lead to THA in JIA patients with HOA.
Methods: 753 patients aged 2-17 years were included in our retrospective study during the last 10 years. Diagnosis was made according to ILAR criteria. Clinical, laboratory and radial examinations were evaluated. Diagnosis of HOA was made on MRI, CT and planar radiograms and confirmed by morphological examination of removed femoral heads.
Results: Total 153/753 (20.3%) patients with JIA had hip involvement. HOA developed in 48/153 (31.4%) of JIA patients and 16/48 (33.3%) of them had THA was undergone. Prevalence of HOA and THA (%) in JIA subtypes: in polyarticular (5/32 (15.6%) and 8/16 (50%), systemic (6/32 (18.7%) and 5/16 (31.2%)), enthesitis-related (19/32 (59.4%) and 3/16 (18.8%)) and psoriatic (2/32 (6.7%) and 0/16) subtypes respectively, р=0,0000001. Patients who underwent THA initially had higher level of inflammation: elevated ESR (33 vs 5 mm/h, p=0.002) and CRP (14.7 vs 1.9 mg/l, p=0.03), more active joint, and especially involvement of joints of upper limbs: elbows (p=0.004) and proximal interphalangeal joints (p=0.001), arthritis of subtalar joint (p=0.02). Delayed biologic treatment (7.5 vs 3.4 years, p=0.043) and delayed achievement of remission (9.2 vs 5.6 years, p=0.047) were main predictors of THA. Patients with HOA without biologics had increased cumulative probability of THA: HR=1.99 (1.01; 3.98), p=0.049 (
Cumulative probability of THA in JIA patients with hip osteoarthritis.
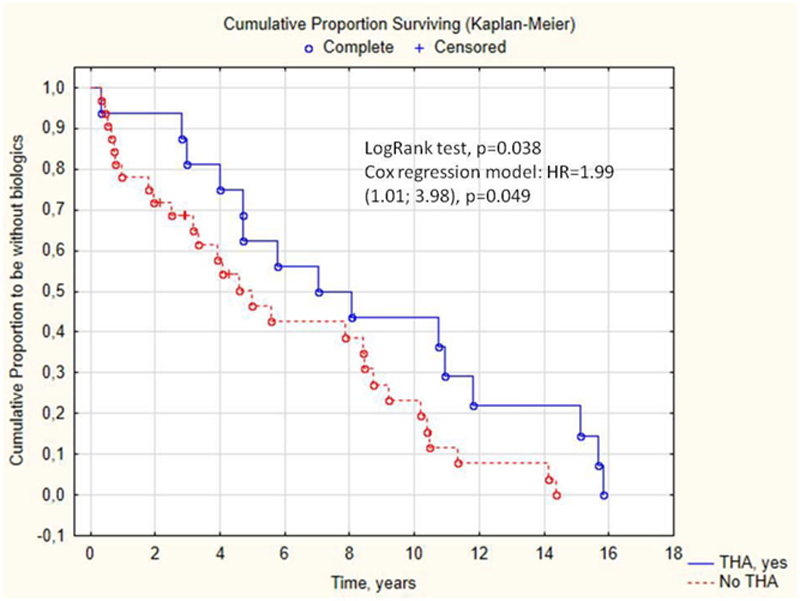
Conclusion: the main risk factors of THA are systemic and polyarticular course because of their activity, systemic CS and delayed biologic treatment. Corticosteroids should be avoided in those group of patients because of risk of avascular pathway HOA formation.
This work supported by the Russian Foundation for Basic Research (grant № 18-515-57001).
The features of JIA patients with hip osteoarthritis depending on
| JIA features | THA, (n=16) | HOA without THA, (n=32) | p |
| Time to THA, years | 5.2 (3.6; 10.2) | 4.6 (2.2; 8.7) | 0.4 |
| Onset age, years | 7.95 (3.5; 11.1) | 8.3 (4.3; 13.1) | 0.5 |
| JIA duration, years | 8.5 (6.5; 13.2) | 5.43 (2.8; 11.1) | 0.07 |
| Polyarticular JIA, n (%) | 8 (50.0) | 5 (15.6) | 0.037 |
| Systemic JIA, n (%) | 5 (31.3) | 6 (7.0) | 0.037 |
| ANA, n (%) | 3/8 (37.5) | 5/16 (31.3) | 0.760 |
| HLA B27, n (%) | 3/6 (50) | 9/19 (47.4) | 0.911 |
| RF, n (%) | 0/9 (0) | 1/15 (6.7) | 0.429 |
| Uveitis, n (%) | 1/16 (6.3) | 3/24 (12.5) | 0.519 |
| ESR, mm/h | 33 (13; 54) | 5 (3; 27) | 0.002 |
| CRP, mg/l | 14.7 (2.9; 72.3) | 1.9 (0.3; 12.7) | 0.03 |
| Active joints, n | 21.5 (8.5; 52.5) | 9 (5; 16) | 0.02 |
| Elbows, n (%) | 11 (68.7) | 8 (25.0) | 0.004 |
| Proximal interphalangeal joints, n (%) | 10 (62.5) | 5 (15.6) | 0.001 |
| Subtalar, n(%) | 4 (25.0) | 1 (3.1) | 0.02 |
| Pulse-therapy GCS, n(%) | 11 (68.7) | 10 (31.3) | 0.014 |
| Cumulative GCS dose, mg | 5000 (3000; 14000) | 4500 (500; 20000) | 0.54 |
| Time to biologic, years | 7.6 (4.3; 11.4) | 3.4 (1.9; 8.6) | 0.04 |
| Achievement of remission, years | 9.2 (6.6; 15.4) | 5.6 (3.3; 11.4) | 0.047 |
Disclosure of Interests: None declared