

Background: Gout is the most common inflammatory rheumatism of industrials countries and chronic renal deficiency is one of the most usual risk factor(1). Uncontrolled gout can cause articular impairment but is also associated with a global and cardiovascular excess mortality, especially in dialysis population(2). International guidelines on gout management remain currently unclear for this particular population(3,4) and current literature data are contradictory on the effectiveness of hemodialysis alone in stemming gout flares.
Objectives: The objective of this study was to analyze the rate of gout flares, during 5 years on gouty patients who starts hemodialysis, treated or not by hypouricemic drugs.
Methods: We performed an observational, retrospective and multicentric study on gouty patients who started hemodialysis between 2005 and 2015 in two nephrology unit.
We recorded demographic, clinical and therapeutic data at the start of hemodialysis and throughout 5 years of follow up.
A gout flare was defined as presence of uric acid crystal in articular punction when it was performed, or clinical diagnosed as such with a colchicine prescription. The effectiveness of dialysis was measured by the KT/V ratio measured during gout flares and 3 times per year for each patient correlated with the serum uric acid level.
According to the French legislation, no ethics committee approval was requested for such a retrospective survey.
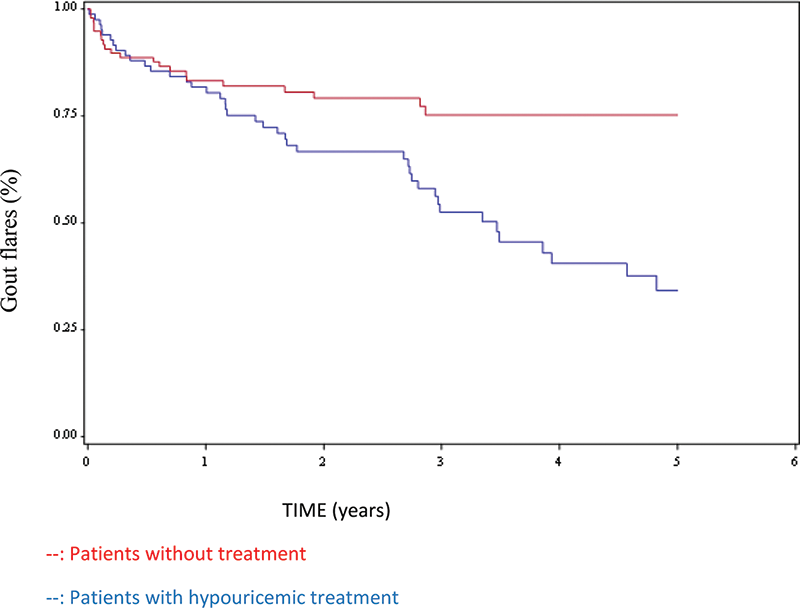
Survival analysis by Kaplan - Meier method and bivariate analysis have been performed to study gout flares and their association with clinical or biological factor.
Results: One hundred eighty two patients have been included, 98/182 (53, 8%) had long term hypouricemic treatment: 88/98 (89%) by allopurinol and 10/98 (11%) by febuxostat.
Mean age at dialysis initiation was 68.6 years with a male/female sex ratio of 2.7:1.
Sixty-four/182 patients (35.16%) presented at least one gout flare during the follow-up: 42 patients (65%) without hypouricemic treatment and 22 patients (45%) with hypouricemic treatment. Patients on hypouricemic treatment since hemodialysis beginning had significantly less gout flares compared to those without (p = 0.0009)
(graphic 1).
There was no significant KT/V ratios difference between the 2 populations at the time of gout flares. Hypouricemic treatment was a protective factor for the occurrence of gout attacks (HR: 0.42, 95% CI 0.25 – 0.71) (
Associated factor of gout flares after the beginning of hemodialysis on gouty patients
| HR | 95% CI | |
|---|---|---|
| Current or active smoking | 0.92 | 0.46-1.86 |
| Male | 0.82 | 1.48-1.42 |
| Caucasian ethnic | 0.83 | 0.64-1.75 |
| Hypouricemic treatment | 0.42 | 0.25-0.71 |
| High Blood Pressure | 1.21 | 0.44-3.36 |
| Obesity | 0.84 | 0.47-1.51 |
| Dyslipidemia | 0.79 | 0.47-1.30 |
| Diabetes | 1.28 | 0.78-2.11 |
| Cardiac failure | 1.42 | 0.73-2.81 |
HR: Hazard Ratio; CI: Confidence interval
Conclusion: Therefore hypouricemic treatment at the initiation of hemodialysis seems to be a protective factor against gout flares, which may persist in dialysis patients. Prospectives studies should be performed to confirm these results for this particular gouty population.
REFERENCES:
[1]Dehlin M, Jacobsson L, Roddy E. Global epidemiology of gout: prevalence, incidence, treatment patterns and risk factors. Nat Rev Rheumatol. 2020 Jul;16(7):380–90.
[2]Jaffe DH, Klein AB, Benis A, Flores NM, Gabay H, Morlock R, et al. Incident gout and chronic Kidney Disease: healthcare utilization and survival. BMC Rheumatol. 2019;3:11.
[3]Richette P, Doherty M, Pascual E, Barskova V, Becce F, Castañeda-Sanabria J, et al. 2016 updated EULAR evidence-based recommendations for the management of gout. Ann Rheum Dis. 2017 Jan 1;76(1):29–42.
[4]FitzGerald JD, Dalbeth N, Mikuls T, Brignardello-Petersen R, Guyatt G, Abeles AM, et al. 2020 American College of Rheumatology Guideline for the Management of Gout. Arthritis Care Res. 2020;72(6):744–60.
Graphic 1. Survival analysis of gout flares
TIME (years)--: Patients without treatment--: Patients with hypouricemic treatment
Disclosure of Interests: None declared