

Background: The risk of acquiring COVID-19, and the severity of illness if acquired, in the context of immune-mediated inflammatory diseases (IMIDs) and their therapy, remains incompletely understood. Reported infection rates and outcomes have varied depending on the IMIDs being studied, the nature and size of the study population, and the presence or absence of appropriate control populations. Having more reliable analysis on larger populations is essential for current and future pandemics.
Objectives: Health records from one of the largest health systems in the US are analyzed to determine whether specific IMIDs, including common rheumatologic conditions and specific immunomodulatory drugs, are associated with certain COVID-19 outcomes, using multivariate models that include common chronic comorbidities.
Methods: Patients (pts) with and without IMIDs who were tested for SARS-CoV-2 antigen (n=1,101,431) were identified from the EHR from Providence St. Joseph Health, which serves much of the western US. Immunomodulatory drug therapy was defined as use within three months prior to the first test. Multivariate logistic regression (LR) was applied with machine learning metrics (feature importance, p-value) reported on an 80% training set and AUROC reported on 20% test set.
Results: Rates for positive COVID-19 tests, invasive mechanical ventilation (IMV) and mortality were not greater in the IMID than non-IMID population, whilst hospitalization was similar (
COVID-19 test results, hospitalization, invasive mechanical ventilation, and mortality
| Tested for COVID | COVID+ | Hospitalized n , % of COVID+ | IMV n , % of COVID+ | Mortality % of COVID+ | |
|---|---|---|---|---|---|
| n (% ) | n , % of tested | n , % of COVID+ | |||
| All pts | 1,101,431 (100%) | 128,962 (11.7%) | 19,704 (15.3%) | 1,001 (0.8%) | 2,232 (1.7%) |
| Pts without selected IMIDs | 1,049,007 (95.3%) | 123,943 (11.8%) | 18,729 (15.1%) | 959 (0.8%) | 2,165 (1.7%) |
| Pts with selected rheumatologic IMIDs | 28,411 (2.5%) | 2,974 (10.5%) | 578 (19.4%) | 27 (0.9%) | 51 (1.7%) |
| Pts with other selected IMIDs | 24,013 (2.2%) | 2,045 (8.5%) | 397 (19.4%) | 15 (0.7%) | 16 (0.8%) |
Selected rheumatologic IMIDs = RA, SpA, PsA, SLE, PsO, SSc; Other selected IMIDs = IBD, MS.
Odds ratio (OR) for selected risk factors for COVID-19 positive test, hospitalization, IMV, and mortality
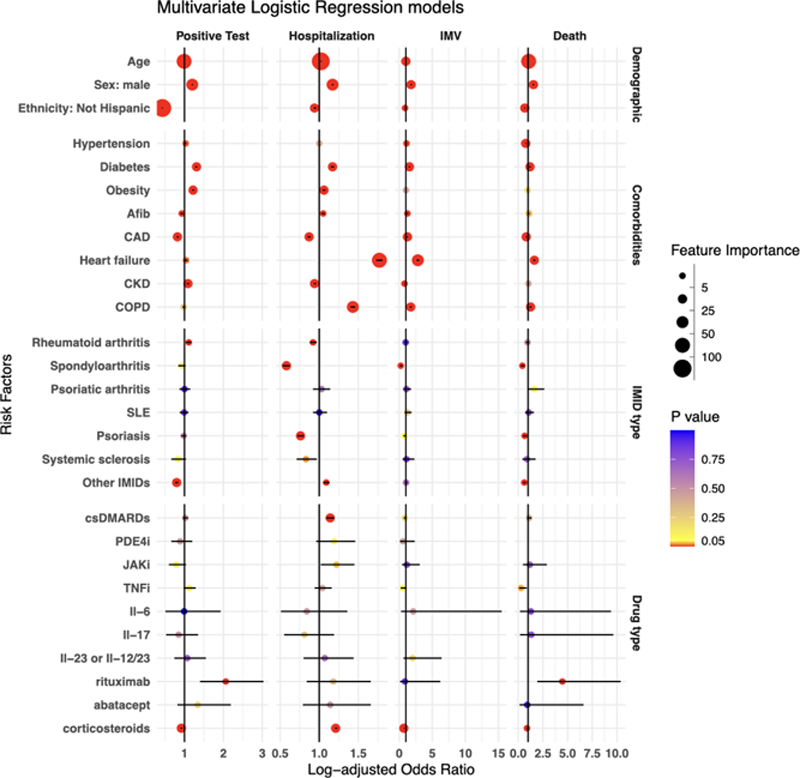
Conclusion: This analysis of COVID+ patients (n=1,101,431) from a large US health care system analyzes outcomes of patients with and without IMIDs; the majority were rheumatologic IMIDs. Patients with IMIDs had a similar rate of hospitalization, IMV, and death as those without IMIDs. The strongest associations with COVID-19 severity included heart failure and age. Spondyloarthritis was weakly associated with favorable outcomes whilst other conditions, including rheumatologic, were not worse than those of non-IMID patients. csDMARDs and corticosteroids were weakly associated with hospitalization and RTX with increased mortality. Other therapies were not associated with severe adverse outcomes.
Acknowledgements: Philip Mease and Qi Wei contributed equally and share first authorship. Swedish Medical Foundation and Pfizer investigator-initiated study grant.
Disclosure of Interests: Philip J Mease Speakers bureau: AbbVie, Amgen, Eli Lilly, Janssen, Novartis, Pfizer, UCB, Consultant of: AbbVie, Aclaris, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly, Galapagos, Gilead, GlaxoSmithKline, Inmagene, Janssen, Novartis, Pfizer, Sun Pharma, UCB, Grant/research support from: AbbVie, Amgen, Bristol Myers Squibb, Eli Lilly, Galapagos, Gilead, Janssen, Novartis, Pfizer, Sun Pharma, Swedish Medical Foundation, UCB, Qi Wei Grant/research support from: Pfizer, Swedish Medical Foundation, Michael Chiorean Speakers bureau: Pfizer, BMS, Takeda, AbbVie, Janssen, Medtronic, Consultant of: Pfizer, Lilly, Janssen, Arena, Medtronic, BMS, AbbVie, Grant/research support from: Takeda, Pfizer, Novartis, Swedish Medical Foundation, Lulu Iles-Shih Grant/research support from: Pfizer, Swedish Medical Foundation, Jennifer Hadlock Grant/research support from: Pfizer, Swedish Medical Foundation