

Background: Dermatomyositis (DM) patients have fewer risks of COVID-19 infection compared to the general population, however, certain subgroups with DM have worse outcomes. Men. African Americans, those with interstitial lung disease, exhibited higher risks of severe COVID-19. DMARD and glucocorticoid use was associated with frequent hospitalisations and severe sepsis.
Objectives: Rheumatic diseases (RDs) like DM, are previously known to be vulnerable towards various types of infections due to its aggressive activity mandating high dose immunosuppressive therapy. The severity of COVID-19 in RDs is limited in literature due to the heterogeneous nature of the condition. Therefore, specific details on mortality is essential to navigate any precautions required in the treatment.
Methods: Retrospective data of individuals with DM and COVID-19 and the general population with COVID-19 between January 2020 to August 2020 was retrieved from the TriNetX database. A one-to-one matched COVID-19 positive control was selected using propensity score (PS) matching. We assessed COVID-19 outcomes such as mortality, hospitalisation, ICU admission, severe COVID-19, mechanical ventilation (MV), acute kidney injury (AKI), venous thromboembolism (VTE), ischemic stroke, acute respiratory distress syndrome (ARDS), renal replacement therapy (RRT) and sepsis. Subgroup analyses included gender, race, ILD, cancer patients, disease-modifying rheumatic drugs (DMARDs) use, and glucocorticoids (GC) use (
Overview of study
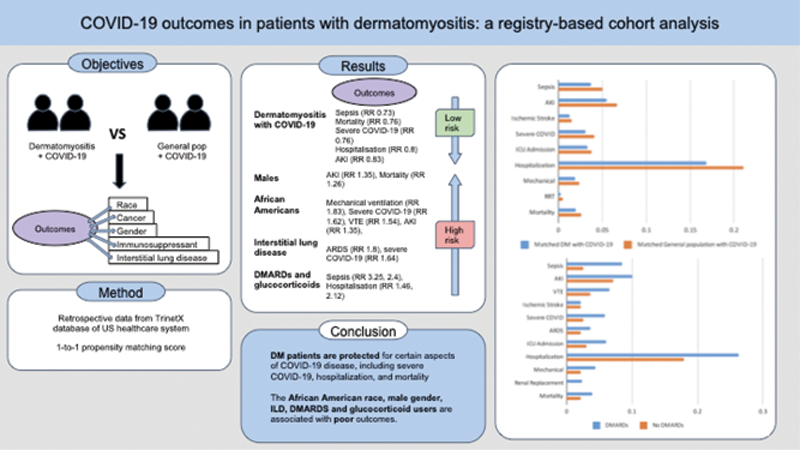
Results: We identified 5,574 DM patients with COVID-19, and 5,574 general population with COVID-19 (controls). DM with COVID-19 had a lower risk of mortality in comparison to controls [RR 0.76], hospitalisation [RR 0.8], severe COVID-19 [RR 0.76], AKI [RR 0.83], and sepsis [RR 0.73]. Males and African Americans were more likely to develop AKI [RR 1.35, 1.65], while African Americans had higher odds for severe COVID-19 [RR 1.62] and VTE [RR 1.54]. DM with ILD group also experienced higher odds for severe COVID-19 infection [RR 1.64], and VTE [RR 2.06] (
DM patients receiving DMARDs and glucocorticoids had higher odds for hospitalisation [RR 1.46, 2.12], and sepsis [RR 3.25] Subgroup analysis of neoplasms amongst DM patients with COVID-19 was inadequate for meaningful comparison (
Conclusion: DM patients are protected for certain aspects of COVID-19 disease, including severe COVID-19, hospitalization, and mortality. The African American race, male gender, ILD, DMARDS and glucocorticoid users, are associated with poor outcomes.
Disclosure of Interests: Latika Gupta: None declared, Haig Pakhchanian: None declared, Hiba Khan: None declared, Rahul Raiker: None declared, Maryam Abbasi: None declared, Charles DeYoung: None declared, Sinan Kardes Grant/research support from: SK has received congress travel, accommodation, and participation fee support (12th Anatolian Rheumatology Days) from Abbvie, Sakir Ahmed Speakers bureau: SA has received honorarium as speaker for Pfizer, Chengappa Kavadichanda: None declared, Parikshit Sen: None declared, Rohit Aggarwal Consultant of: RA has/had a consultancy relationship with and/or has received research funding from the following companies-Bristol Myers-Squibb, Pfizer, Genentech, Octapharma, CSL Behring, Mallinckrodt, AstraZeneca, Corbus, Kezar, and Abbvie, Janssen, Alexion, Argenx, Q32, EMD-Serono, Boehringer Ingelheim, Roivant., Grant/research support from: RA has/had a consultancy relationship with and/or has received research funding from the following companies-Bristol Myers-Squibb, Pfizer, Genentech, Octapharma, CSL Behring, Mallinckrodt, AstraZeneca, Corbus, Kezar, and Abbvie, Janssen, Alexion, Argenx, Q32, EMD-Serono, Boehringer Ingelheim, Roivant.