

Background: ANCA-associated vasculitis (AAV) are small vessel vasculitis which may variously affect upper and lower respiratory tract. Patients with microscopic polyangiitis (MPA) and, less commonly, granulomatosis with polyangiitis (GPA), especially those who are ANCA-MPO-positive, may suffer from interstitial lung disease (ILD), which is associated with high morbidity and mortality as it is often underdiagnosed and responds poorly to conventional treatments
Objectives: In this study, we aimed to assess whether Krebs von den Lungen-6 (KL-6), a marker of fibrotic ILD, may be useful for distinguishing AAV patients with ILD from those without ILD, and whether its changes over time are correlated with disease activity.
Methods: We enrolled all consecutive patients evaluated in the period December 2020 - November 2021. Inclusion criteria were a diagnosis of GPA or MPA, active disease, and eligibility for Rituximab treatment according to EULAR recommendations. All patients underwent concomitant rheumatological and pneumological evaluation, lung function tests, routine blood tests, autoimmunity evaluation and KL-6 assay. Current and previous treatments, Birmingham vasculitis score (BVAS) and vasculitis damage index were also recorded.
Results: A total of 13 patients (
Patients’ features
| Sex/age | Diagnosis | Length of disease * (months) | Organs involved | Type of lung involvement | T0 KL6 levels | T0 BVAS | T0 VDI | T1 KL6 levels | T1 BVAS | T1 VDI |
|---|---|---|---|---|---|---|---|---|---|---|
| F/83 | MPA | 28 | Lung, kidney, PNS | ILD, alveolar hemorrhage | 625 | 8 | 7 | 325 | 0 | 7 |
| M/48 | GPA | 1 | Lung, kidney, nose, eye | Nodules | 352 | 18 | 0 | 279 | 2 | 0 |
| F/55 | GPA | 252 | Lung, skin | Nodules | 401 | 15 | 3 | 602 | 3 | 3 |
| F/38 | MPA | 1 | Skin | - | 347 | 6 | 0 | - | - | - |
| F/74 | MPA | 180 | Kidney, PNS | - | 368 | 11 | 5 | 414 | 0 | 5 |
| M/77 | MPA | 8 | Lung, kidney, PNS, skin | ILD, alveolar hemorrhage | 982 | 24 | 1 | - | - | - |
| F/49 | GPA | 60 | Nose, eye | - | 122 | 6 | 2 | 116 | 0 | 2 |
| M/60 | MPA | 40 | Skin, PNS | - | 205 | 9 | 1 | - | - | - |
| F/39 | GPA | 4 | Nose | - | 310 | 6 | 3 | - | - | - |
| M/71 | GPA | 24 | Lung, eye, joints | Nodules, ILD | 1528 | 9 | 3 | - | - | - |
| F/64 | MPA | 24 | Lung | ILD | 756 | 4 | - | 1003 | 0 | - |
| F/59 | GPA | 72 | Lung | Nodules | 338 | 4 | - | - | 0 | - |
ROC curve and decision tree model
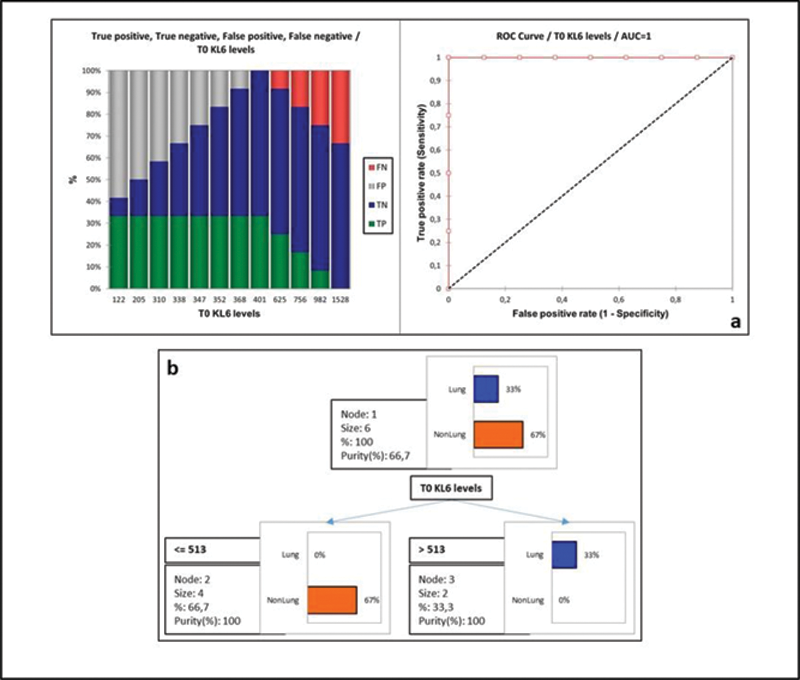
Conclusion: Our multicentre study demonstrated KL-6 as a reliable, non-invasive and easy-to-perform marker of ILD in AAV patients and its helpfulness for disease activity assessment. Changes in serum concentrations of KL-6 over time could be useful for monitoring AAV patients. Further study of KL-6 as a marker of response to therapy during long-term follow-up would also be worthwhile.
Disclosure of Interests: None declared