

Background: Ocular and Neurobehçet’s Disease (NBD) are the most severe manifestations of Behcet’s disease (1-4 ). NBD can be classified as a ) primary neural parenchymal lesions, also known as parenchymal NBD (p-NBD) or b ) secondary to vascular involvement or non-parenchymal NBD (np-NBD) (4 ). Response to biologic therapy (BT) in these two refractory subtypes of NBD is unknown.
Objectives: To assess efficacy and safety of BT in refractory subtypes of NBD.
Methods: Open-label multicenter study of refractory NBD from 21 different referral National Hospitals. NBD diagnosis was based on the International Consensus Recommendation criteria (4 ). Efficacy was determined by complete or partial response and no-response. Complete, partial or no response was defined according to the resolution of the neurological syndrome (signs and/or symptoms) after the BT onset.
Results: We studied 41 patients (21 women/20 men; mean age: 40.6±10.8 years). NBD was classified as p-NBD (n= 33, 80.5%) and np-NBD (n=17, 41.5%). There were no significant differences in baseline general features and in neurological clinical response in both subgroups (
Main features of p-NBD and np-NBD
| Total | p-NBD | np-NBD | P p-NBD vs np-NBD | |
|---|---|---|---|---|
| Age at biological therapy initiation, years (mean±SD ) | 44±13.9 | 41.4±9.6 | 39.4±10.6 | 0.412 |
| Gender, n (m/f) (% ) | 21/20 (48.8/52.2) | 18/15 (54.5/45.5) | 5/12 (29.4/70.6) | 0.091 |
| HLAB51 +/ patients tested, n (% ) | 15/31 (57.7) | 14/25 (58.3) | 4/10 (40) | 0.391 |
| Oral aphthae, n (% ) | 40 (97.6) | 32 (97) | 15 (88.2) | 0.323 |
| Cutaneous involvement, n (% ) | 28 (63.4) | 23 (69.7) | 10 (58.8) | 0.603 |
| Ocular involvement, n (% ) | 21 (48.8) | 15 (45.5) | 9 (52.9) | 0.616 |
| Vascular involvement, n (% ) | 9 (22) | 10 (30.3) | 7 (41.2) | 0.442 |
| Articular involvement, n (% ) | 9 (22) | 7 (21.2) | 3 (17.6) | 0.765 |
| Previous conventional Immunosuppressive drugs to BT | ||||
| Azathioprine | 24 (58.5) | 20 (60.6) | 10 (58.8) | - |
| Methotrexate | 16 (39.0) | 12 (36.4) | 3 (17.6) | - |
| Cyclophosphamide | 13 (31.7) | 13 (39.4) | 5 (29.4) | - |
| Cyclosporine A | 9 (22.0) | 8 (24.2) | 3 (17.6) | - |
| Mycophenolate Mofetil | 2 (4.9) | 2 (6.1) | 0 | - |
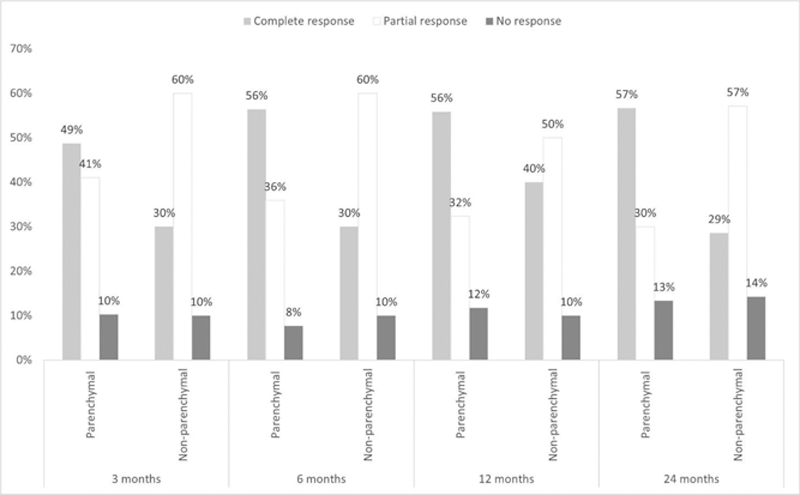
Response to biological therapy according to NBD subtypes.
After an overall mean follow-up of 57.5±50.9 months BT was switched in 22 patients due to inefficacy (n=16) or Adverse Effects (AE) (n=6) and in 4 cases was definitively discontinued because of complete prolonged remission (n=3) or AE (n=1). AE were observed in 7 (17.1%) patients. Severe AE were observed in 2 cases, one due to demyelinating disease and the other due to pulmonary tuberculosis, both in patients undergoing IFX therapy. The other 6 AE were infusion reaction to IFX (n=1), IFX-induced psoriasis (n=1), IFX-induced acneiform eruption (n=1), infusion reaction to TCZ (n=1), intolerance to IFX and recurrent mild infections (n=1) and erosive lichen planus and bullous impetigo (n=1).
Conclusion: In our series, BT seems equally effective and safe in both refractory p-NBD and np-NBD.
REFERENCES:
[1]Martín-Varillas JL, et al. Ophthalmology 2018 Sep;125(9):1444-1451. doi: 10.1016/j.ophtha.2018.02.020.
[2]Atienza-Mateo B, et al. Arthritis Rheumatol 2019 Dec;71(12):2081-2089. doi: 10.1002/art.41026.
[3]Santos-Gómez M, et al. Clin Exp Rheumatol 2016 Sep-Oct;34(6 Suppl 102): S34-S40.
[4]Kalra S, et al. Diagnosis and management of Neuro-Behçet’s disease: international consensus recommendations. J Neurol. 2014 Sep;261(9):1662–76.
Disclosure of Interests: Alba Herrero-Morant: None declared, José Luis Martín-Varillas Grant/research support from: AbbVie, Pfizer, Lilly, Janssen, UCB, and Celgene, Santos Castañeda Paid instructor for: Assistant professor of the Cátedra UAM-ROCHE, EPID-Future, UAM, Madrid, Spain, Olga Maiz-Alonso: None declared, Julio Sanchez-Martin: None declared, Norberto Ortego: None declared, Enrique Raya: None declared, Águeda Prior-Español: None declared, Clara Moriano: None declared, Rafael Melero: None declared, Jenaro Graña: None declared, ANA URRUTICOECHEA-ARANA: None declared, Angel Ramos Calvo: None declared, Marta Loredo Martínez: None declared, Eva Salgado-Pérez: None declared, Francisca Sivera: None declared, Ignacio Torre-Salaberri: None declared, J. Narváez Speakers bureau: Bristol-Myers Squibb, José Luis Andréu Sánchez: None declared, Olga Martínez González: None declared, Ricardo Gómez de la Torre: None declared, Sabela Fernández: None declared, Susana Romero-Yuste: None declared, Iñigo Gonzalez-Mazon: None declared, Carmen Álvarez-Reguera: None declared, David Martínez-López: None declared, J. Luis Hernández: None declared, Miguel Á. González-Gay Speakers bureau: Abbvie, Roche, Sanofi, Lilly, Celgene, Sobi, and MSD, Grant/research support from: Abbvie, MSD, Janssen, and Roche, Ricardo Blanco Speakers bureau: Abbvie, Lilly, Pfizer, Roche, BMS, Janssen, and MSD, Grant/research support from: Abbvie, MSD, and Roche