

Background: The idiopathic inflammatory myopathies (IIMs) are a heterogeneous group of diseases that can affect the muscles, skin, lungs, heart, and joints. Increase knowledge about histopathological findings, clinical manifestations and auto-antibodies have allowed further novel classification of IIMs. Today, the main IMs subgroups are: dermatomyositis (DM), inclusion body myositis (IBM), immune-mediated necrotizing myopathies (IMNM), overlap myositis (OM) and immune-checkpoint inhibitor-related myositis (ICIrm). Axial muscle involvement results either in a “Dropped Head Syndrome (DHS)”, with a marked weakness of the neck extensors, or in a camptocormia (CC), with a weakness of the thoracolumbar paraspinal muscles. This atypical presentation is poorly described in the course of IMs while it may results in a major disability, and may lead to myositis diagnosis delay.
Objectives: This study aimed to describe IMs revealed by DHS and/or CC. Secondary outcomes were to define subgroups of patients according to clinical, biological and histopathological characteristics. Then, the effects of treatments used were analyzed.
Methods: A historical cohort was designed using the register MYOLYON which includes all IMs followed at the University Hospital of Lyon (France) between 2000 and 2021. All patients with IM revealed by DHS and/or CC and having an histologically proven IMs were included, after exclusion of alternative (e.g., myasthenia gravis, motoneuron disease). Clinical, biological, immunological, histopathological data as well as outcome and care were collected through a standardized form. Agreement for the study was obtained from the French Ministry of the Research and the study was approved by the Local Research Ethics Committee.
Results: Twenty-two patients were fully characterized: DM (n=4), IBM (n=7), OM (n=8), ICIrm (n=2) and one myositis with anti-Hu antibodies. Two groups of patients were identified according to the age at first symptoms and to the type of muscle axial involvement (e.g, DHS and/or CC). Before the age of 70 (n=13/22), the two most common diagnoses (n=11/13) were DM (n=4/4) and OM (n=7/8). Axial muscle involvement was diffuse (DHS and CC) in 10/13 patients. After 70 years old (n=9/22), there were a majority of IBM (n=6/9) and all cases of ICIrm (n=2). Axial involvement was restricted to one group of muscles (DHS or CC) in 5/9 patients. Finally, 77% (17/22) of patients had refractory disease and required a second line treatment (e.g, immunoglobulins). All of these results are summarized in the
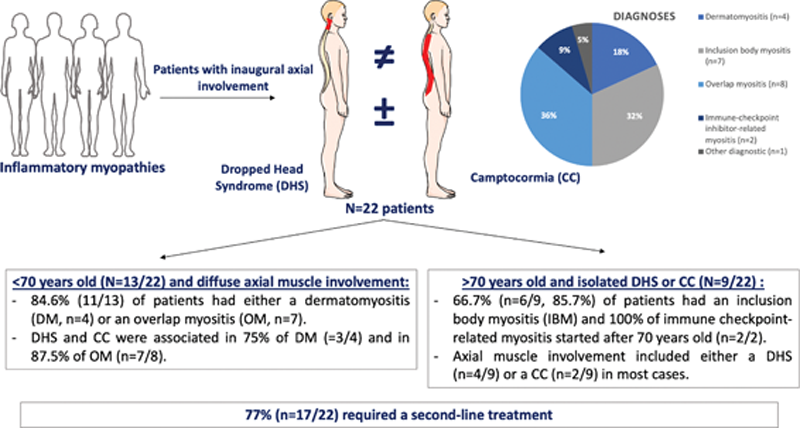
Conclusion: While IM diagnosis is challenging in the presence of inaugural axial involvement, these results highlight the subset of IM to be considered according to the age at first symptoms and the type of axial involvement (e.g., DHS and/or CC).
REFERENCES:
[1]Mariampillai, K. et al. Development of a New Classification System for Idiopathic Inflammatory Myopathies Based on Clinical Manifestations and Myositis-Specific Autoantibodies. JAMA Neurol 75 , 1528-1537 (2018).
[2]Landon-Cardinal, O. et al. Recognising the spectrum of scleromyositis: HEp-2 ANA patterns allow identification of a novel clinical subset with anti-SMN autoantibodies. RMD Open 6 (2020).
[3]Suarez, G.A. & Kelly, J.J., Jr. The dropped head syndrome. Neurology 42 , 1625-1627 (1992).
[4]Oerlemans, W.G. & de Visser, M. Dropped head syndrome and bent spine syndrome: two separate clinical entities or different manifestations of axial myopathy? J Neurol Neurosurg Psychiatry 65 , 258-259 (1998).
Disclosure of Interests: None declared