

Background: In radiographic axial spondyloarthritis (r-axSpA) it has been hypothesized that inflammation-driven bone loss triggers bone repair at anatomically distinct sites of the same vertebra: bone loss occurring in the trabecular bone and ectopic bone formation in the periosteum 1 .
Objectives: To investigate whether inflammation is associated with lower bone density (surrogate of bone loss) and subsequently, if lower bone density is associated with 2-year bone formation in r-axSpA at the same vertebra.
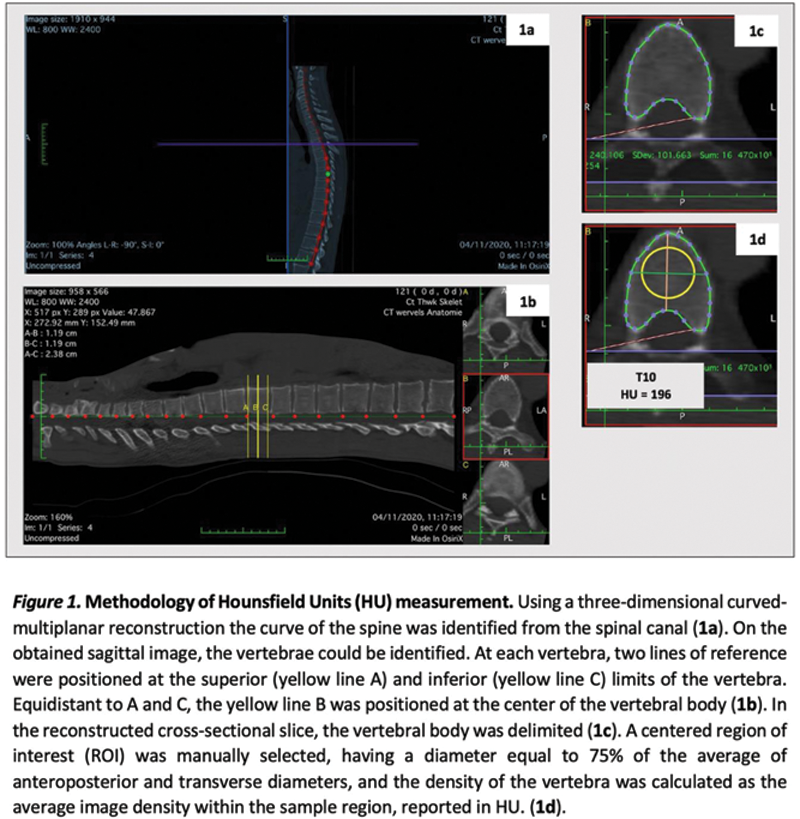
Methods: Data from the Sensitive Imaging in Ankylosing Spondylitis (SIAS), a multicentre 2-year cohort, was used. Baseline vertebral bone density was assessed by Hounsfield Units (HU) on low dose Computed Tomography (ldCT) by two independent readers (
Results: We analysed 1,100 vertebrae in 50 patients with r-axSpA. Intraclass correlation coefficients for HU measurements varied from 0.89 to 0.97, Fleiss Kappa values for MRI-BME were between 0.41-0.78 and Cohen´s kappa for syndesmophyte formation/growth change scores varied from 0.36 to 0.74. Bone density HU decreased from cranial to caudal vertebrae. Baseline MRI-BME was present in 300/985 (30%) and syndesmophytes in 588/910 (65%) vertebrae, both most prevalent at the thoracolumbar region. Syndesmophyte formation or growth was observed in 18% of at-risk vertebrae (124/691). A significant association was found between inflammation (MRI-BME) and lower bone density (regression coefficient=-51; 95% CI:-63;-39) (
Relationships between (A) baseline MRI detected spinal inflammation (MRI-BME) and bone density, and (B) baseline bone density and ldCT bone formation after two years, at the same vertebra.
| A. | Independent variables | Bone density (Hounsfield Units ) | |
|---|---|---|---|
| Univariable analysis | Multivariable analysis | ||
| Reg coeff. (95% CI) | Adj Reg coeff. (95% CI) | ||
| N = 910 to 985 | N = 985 | ||
| MRI-BME (presence) | -51 (-63 to -39 ) | -51 (-63 to -39 ) | |
| Age (years) | -1 (-2 to 1) | -1 (-2 to 1) | |
| Gender (male) | 21 (-20 to 63) | 16 (-24 to 57) | |
| TNFi treatment (yes) | 26 (-7 to 59) | 27 (-6 to 61) | |
| Baseline syndesmophytes (presence)* | -42 (-54 to -30 ) | - | |
| B. | Independent variables | Syndesmophyte formation or growth§ | |
| Univariable analysis | Multivariable analysis | ||
| OR (95% CI) | AdjOR (95% CI) | ||
| N = 672 to 691 | N = 672 | ||
| Bone density (HU) | 1.00 (0.99 to 1.00) | 1.00 (0.99 to 1.00) | |
| Age (years) | 1.02 (0.99 to 1.06) | 1.02 (0.98 to 1.05) | |
| Gender (male) | 0.44 (0.13 to 1.52) | 0.56 (0.15 to 2.06) | |
| Smoking (current) | 0.89 (0.40 to 1.97) | 1.02 (0.42 to 2.44) | |
| Treatment with TNFi (yes) | 1.34 (0.56 to 3.21) | 1.30 (0.43 to 3.90) | |
| MRI-BME (presence) | 2.03 (1.23 to 3.71 ) | 1.73 (1.06 to 3.34 ) | |
| Baseline syndesmophytes (presence)* | 2.84 (1.83 to 4.41 ) | - | |
*Multicollinearity with MRI-BME. § Absolute agreement of readers.
adjOR - adjusted odds ratio; CI -confidence interval; BME - bone marrow edema; HU - Hounsfield units; ldCT - low dose computed tomography; MRI - magnetic resonance imaging; TNFi – Tumour necrosis factor inhibitors. Statistical significance highlighted in bold.
Conclusion: While in r-axSpA vertebral inflammation associates with low vertebral bone density, lower vertebral bone density itself does not increase the risk for ectopic bone formation at the same vertebra.
REFERENCES:
[1]Lories RJ. Best Pract Res Clin Rheumatol. 2018 Jun;32(3):331–41.
Acknowledgements: To the Dutch Rheumatism Association for funding SIAS study.
Disclosure of Interests: Mary Lucy Marques: None declared, Nuno Pereira da Silva: None declared, Désirée van der Heijde Consultant of: AbbVie, Gilead, Glaxo-Smith-Kline, Lilly, Novartis, UCB Pharma, Rosalinde Stal: None declared, Xenofon Baraliakos: None declared, Juergen Braun: None declared, Monique Reijnierse: None declared, Caroline Bastiaenen: None declared, Floris A. van Gaalen: None declared, Sofia Ramiro: None declared