

Background: Gout is a highly prevalent inflammatory arthritis with increasing global disease burden in recent years. 1,2 Gout prevalence has been reported to be higher among Blacks compared to Whites, 3 and that they are less likely to receive allopurinol in outpatient care. 4 The potential nationwide impact of these racial disparities on emergency department (ED) visits and hospitalizations is unknown.
Objectives: To examine the contemporary racial disparities in ED visits and hospitalizations with a primary discharge diagnosis of gout in the US (2019).
Methods: We compared ED visits and hospitalizations between Blacks and Whites in the latest data (2019) from the US National Emergency Department Sample (NEDS) and National Inpatient Sample (NIS). We focused on encounters for which the primary diagnosis was gout based on ICD codes (M1A.xx, M10.xx). We calculated annual population rates of ED visits and hospitalizations for gout (per 100,000 US adults) using the 2019 US census adult population (>18 years) according to race.
Results: There were a total of 160,759 ED visits and 9,560 hospitalizations among White and Blacks with a gout diagnosis in the US in 2019. The mean age (58.2 years vs. 56.5 years) and male proportion (78.0% vs. 74.8%) tended to be higher among Whites, while more Blacks tended to live in the South (40.7% vs. 66.5%) and reported a median household income of < $50,000 (30.7% vs. 57.1%). Compared to Whites, Blacks had 2.7- and 3.2-fold higher rates of gout ED visits and hospitalizations, respectively, after adjusting for age, sex, payer, region, and household income (
Racial Disparities in Emergency Department Visits and Hospitalizations with Primary Diagnosis of Gout in 2019
| Emergency Department Visits | Hospitalizations | |||
|---|---|---|---|---|
| Race | White | Black | White | Black |
| All | 68011965 | 24521330 | 19851043 | 4519150 |
| Visits, N | 88810 | 71949 | 6200 | 3360 |
| Rate per 100,000 | 130.6 | 293.4 | 31.2 | 74.4 |
| Rate Ratio (95% CI)* | 1.0 (ref) | 2.81 (2.63, 3.00 ) | 1.0 (ref) | 3.08 (2.79, 3.40 ) |
| Rate Ratio (95% CI)** | 1.0 (ref) | 2.66 (2.50, 2.82 ) | 1.0 (ref) | 3.17 (2.86, 3.50 ) |
| Women | 37851369 | 14363031 | 11039093 | 2647105 |
| Visits, N | 19567 | 18163 | 1770 | 1145 |
| Rate per 100,000 | 51.7 | 126.5 | 16.0 | 43.3 |
| Rate Ratio (95% CI)* | 1.0 (ref) | 3.68 (3.39, 3.99 ) | 1.0 (ref) | 4.01 (3.40, 4.73 ) |
| Rate Ratio (95% CI)** | 1.0 (ref) | 3.36 (3.11, 3.62 ) | 1.0 (ref) | 4.02 (3.39, 4.78 ) |
| Men | 30156101 | 10156573 | 8809815 | 1871620 |
| Visits, N | 69228 | 53783 | 4430 | 2215 |
| Rate per 100,000 | 229.6 | 529.5 | 50.3 | 118.3 |
| Rate Ratio (95% CI)* | 1.0 (ref) | 2.59 (2.42, 2.78 ) | 1.0 (ref) | 2.66 (2.36, 3.00 ) |
| Rate Ratio (95% CI)** | 1.0 (ref) | 2.47 (2.32, 2.64 ) | 1.0 (ref) | 2.77 (2.45, 3.14 ) |
*Adjusted for age and sex for all, adjusted for age for sex-specific rate ratios
**Adjusted for age, sex, payment, region, and household income
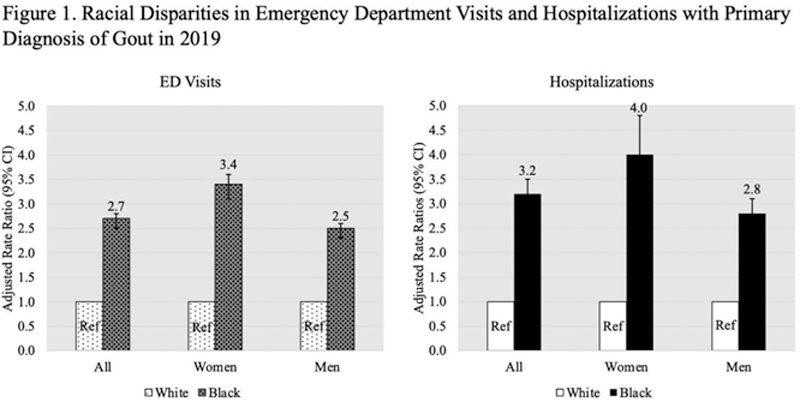
Conclusion: These latest national data indicate that ED visits and hospitalization due to gout are both 3 times higher among Blacks than Whites; this disparity was particularly prominent among women with gout. Higher risk of developing gout 3 and suboptimal care 4 both translate to these avoidable costly healthcare utilizations, calling for improved primary prevention and gout care.
REFERENCES:
[1]Safiri et al., PMID 32755051
[2]Xia et al., PMID 31624843
[3]Chen-Xu et al., PMID 30618180
[4]Krishnan et al., PMID 18260174
Disclosure of Interests: Chio Yokose: None declared, Natalie McCormick: None declared, Na Lu: None declared, Amit Joshi: None declared, Lesley Jackson: None declared, Minna Kohler Speakers bureau: Lilly, Consultant of: Mymee, Novartis, Grant/research support from: Setpoint Medical, Janeth Yinh: None declared, Yuqing Zhang: None declared, Kenneth Saag Consultant of: Arthrosi, Atom Bioscience, Horizon Therapeutics, LG Pharma, Mallinkrodt, SOBI, Takeda, Grant/research support from: Horizon Therapeutics, SOBI, Shanton, Hyon Choi Consultant of: Ironwood, Selecta, Horizon, Takeda, Kowa, and Vaxart, Grant/research support from: Ironwood and Horizon