

Background: Patients with giant cell arteritis (GCA) represent a fragile population with an increased infection risk. In a recent study 1 older age, a higher number of comorbidities, higher disease activity, and prednisolone ≥10 mg qd were associated with worse COVID-19 outcomes.
Objectives: We aimed to evaluate the frequency and severity of COVID-19 in a well-defined GCA cohort.
Methods: We reviewed medical records of histologically and/or by imaging proven GCA patients diagnosed between September 2011 and February 2020 at our secondary/tertiary center and followed during the COVID-19 pandemic between March 2020 and December 2021 (22 months). Descriptive statistics was used to analyze the studied population.
Results: Of 314 GCA patients diagnosed for the first time during a 102-month period, 49 patients died before March 2020. Of the remaining 265 patients (69.4% females), SARS-CoV-2 infection was proven by PCR test in 39 (14.7%) patients (74.2% females, mean (SD) age at infection 76.2 (±9.6 years), 13 (33.3%) with large vessel GCA and 16 with cranial limited GCA). At the time of SARS-Cov-2 infection GCA was in a stable remission in 38 patients (13 without therapy, 10 on steroids alone, 9 on leflunomide monotherapy, 6 on steroids plus leflunomide (10 or 20 mg qd), 1 on ustekinumab; mean prednisolone equivalent dose of 4.6 mg qd) and relapsed in one patient 6 weeks earlier (prednisolone 30 mg plus leflunomide). Data on clinical manifestations of COVID-19 were available for 33 (84.6%) patients and are presented in
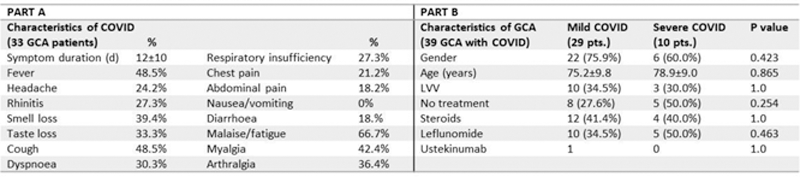
Conclusion: A quarter of our GCA patients had severe COVID-19. Low doses of glucocorticoids and treatment with leflunomide were not associated with severe COVID-19 course in our cohort.
REFERENCES:
[1]Sattui SE, et al. Lancet Rheumatol 2021; doi: 10.1016/S2665-9913(21)00316-7
Disclosure of Interests: None declared