

Background: Polymyalgia rheumatica (PMR) is common in patients over the age of 50 years. Clinical symptoms promptly respond to glucocorticoid therapy, but there are wide variations of dosage tapering, treatment duration and rate of relapses. In Slovenia epidemiology of PMR is unknown.
Objectives: We aimed to determine the incidence rate of PMR, the clinical characteristics, the relapse frequency and length of glucocorticoid therapy.
Methods: A detailed single centre retrospective review of medical records of all patients diagnosed with PMR between 1 January 2014 and 31 December 2016 was performed at the Department of Rheumatology, University Medical Centre Ljubljana, Ljubljana, Slovenia–the only secondary level rheumatology institution in serving the Central Slovenian and Gorenjska regions, which represent ~40% (7×105) of the Slovenian adult population. The outcomes were assessed up to1 October 2021.
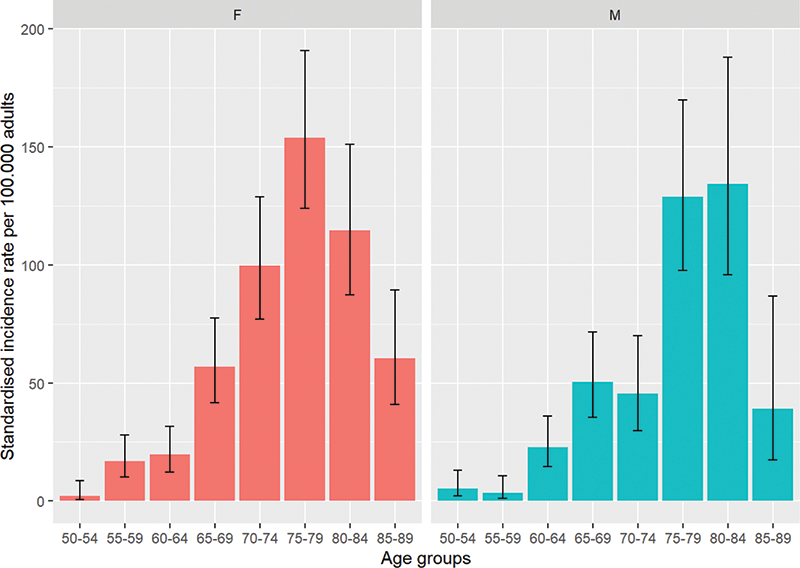
Results: During the 3-year period 494 patients (460 from Ljubljana and Gorenjska regions) were diagnosed with PMR (64% females, median (IQR) age 75 (69, 80) years), resulting in an annual sex- and age-standardised incidence rate (IR) per 105 adults ≥ 50 years of 46.0 (95% CI 42.0, 50.4), with a female/male ratio of 1.5 (95% CI 1.3, 1.7). The IR peaked between 70–85 years (
At presentation, 96% had morning stiffness (71% lasting >45 minutes), 99% shoulder pain, 94% pelvic girdle pain, 49% weight loss, 13% peripheral arthritis, and 12% body temperature >37°C. Data on US of shoulders and hips was complete, partial, or missing for 38%, 24%, 39%, respectively. Elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) was present in 98% of patients, the median (IQR) ESR was 55 (42, 71) and CRP 49 (26, 79) mg/l, and 58% had anaemia. RF and ACPA were positive in 4% and 3%, respectively. 8/12 had ACPA values less than 2× the reference value. During follow-up ACPA was repeated in 8/12 patients and negativized in 6/8 patients. Among other pre-existing conditions, 51 (10%) had history of malignancy diagnosed a median 7 (3–11) years prior to diagnosis of PMR. EULAR/ACR classification criteria for PMR were fulfilled in 68% and 71% based on clinical and extended ultrasound criteria (missing items were imputed with 0), respectively. 14 (3%) patients had clinically overt concurrent giant cell arteritis (GCA).
All patients were treated with methylprednisolone, administered orally in 99.4%, 93% started at 16mg qd. By the end of follow-up, 295 (60%) patients successfully discontinued methylprednisolone after a median of 117 (104, 143) weeks. Steroid sparing leflunomide and methotrexate were used by 66 (13%) and 27 (6%) patients, respectively. During a median follow-up of 150 (98, 244) weeks, 146 (30%) had at least one relapse. Median time to first relapse was 111 (50, 141) weeks. 54% relapsed after glucocorticoid discontinuation after a median time of 4 (2, 18) weeks, 9% presented with GCA, 12% relapsed due to treatment non-adherence. During the follow-up 6% were diagnosed with malignancies.
Conclusion: (1) With the IR of 46 per 105 adults ≥50 years, PMR is more common as rheumatoid arthritis in Slovenia. (2) A considerable proportion of patients required long-term glucocorticoid treatment, leaving a huge unmet need for safer therapeutic options.
Disclosure of Interests: None declared