

Background Chronic inflammation in inflammatory arthritis can trigger both peripheral and central sensitization (CS) through central modifications of pain pathways. CS is an abnormal pain management mechanism involving the central nervous system.
Objectives To evaluate the frequency of CS and neuropathic pain (NP) in patients with psoriatic arthritis (PsA) and its relationship with disease activity and functional status.
Methods Patients classified as PsA according to CASPAR classification criteria were included in this cross-sectional study. Disease activity was evaluated with DAPSA, VAS, pain and fatigue level (0-100 mm), quality of life with HAQ, CS with CS inventory (CSI). A score of 40 point was used to predict the presence of CS. CS score of <30 was also categorized as subclinical, 30 -39 as mild, 40-49 as moderate, 50-59 as severe and ≥60 as extreme. NP was evaluated with the DN4 (Douleur Neuropathique en 4 questions) scale. The presence of anxiety and depression were evaluated by using the Hospital Anxiety and Depression questionnaire (HADS) and fibromyalgia syndrome (FMS) by ACR 2016 criteria.
Results İn total 114 PsA patients (78 [68.4%] female, mean age: 48.8 ±11.6 years, median disease duration was 4 [9] years) were included in the study. The median DAPSA score was 15.2(16), with approximately half of the patients were in remission or low disease activity. The proportion of patients with LEI≥1 was 28.9%, median BSA was 1(2), BASDAI was 3.8(3.6), BASFI was 2[4]. Of our patients 39.8% were receiving biological treatment. 61.4% of the patients had at least one comorbidity.
CS was detected in 49 (42.9%) and NP in 24 (23.7%) patients. The median CSI score was 35.5 (IQR 29) Among patients with CS and NP the percentage of female was higher. DAPSA, PGA, PhGA, Pain VAS, TJC were found to be significantly higher and HAQ scores were found to be worse in patients with CS and NP. In addition,the percentage of patients with a LEI ≥1 was found 44.9% in patients with CS, and body mass index was found to be higher in patients with NP (Table 1). Duration of disease, CRP, ESR, BSA, usage of biological therapy, treatment with GCs, comorbidities were similar between the groups. Anxiety were higher in patient with CS and NP, and depression was higher in only CS patients. While all 11 patients with FMS had NP, only 8 had CS. Sixteen (%32.7) patients with CS also had NP and 16 (66.7%) patients with NP had also CS. The positive correlation between PGA, PhGA, DAPSA, HAQ and CS severity in PsA patients (Figure 1).
Conclusion The results of the present study revealed that both CS and NP are common in PsA, and FMS accompanies 22.4% of those patients. CS and NP affect quality of life and functionality. In PsA patients, especially in cases where treatment goals cannot be achieved, it may be useful to evaluate the presence of concomitant CS and NP.
| Variables | Patient with |
Patient without |
p | Patient |
Patient without |
p |
|---|---|---|---|---|---|---|
| Female gender,n(%) | 38(81.6) | 40(58.5) | 0.008 | 19(90.5) | 45(60) | 0.009 |
| Age,y,mean(SD) | 51(11) | 47.7(11) | 0.439 | 50.1(10) | 48.2(11.6) | 0.487 |
| BMI,kg/m2, median(IQR) | 29.3(8) | 28.2(7.7) | 0.749 | 32.3(9.6) | 26.9(5.9) | 0.011 |
| TJC, median(IQR) | 2(4) | 0(1) | 0.003 | 1(11) | 0(2) | 0.021 |
| SJC, median(IQR) | 0(0) | 0(0) | 0.996 | 0(0) | 0(0) | 0.533 |
| PGA, median(IQR) | 50(48) | 30(20) | <0.001 | 60(60) | 30(25) | <0.001 |
| PhGA, median(IQR) | 20(30) | 20(10) | 0.001 | 30(20) | 20(20) | 0.001 |
| Pain VAS, median(IQR) | 50(38) | 20(30) | <0.001 | 60(60) | 30(50) | <0.001 |
| LEI≥1,n(%) | 22(44.9) | 11(16.9) | 0.001 | 10(41.7) | 19(24.4) | 0.100 |
| DAPSA, n(%) | 17.9(11) | 9.7(11.9) | <0.001 | 20.2(13) | 11.7(11) | 0.003 |
| Biological therapy, n(%) | 18(37.5) | 27(41.5) | 0.712 | 10(41.7) | 27(35.1) | 0.558 |
| HAQ, median(IQR) | 1(0.85) | 0.38(0.75) | <0.001 | 1.38(1.3) | 0.5(0.8) | <0.001 |
| Anxiety, n(%) | 18(40) | 5(8.1) | <0.001 | 9(40.9) | 12(16.2) | 0.020 |
| Depression, n(%) | 15(33.3) | 4(6.5) | <0.001 | 5(22.7) | 11(14.9) | 0.514 |
| FMS, n(%) | 13(35.6) | 8(12.9) | 0.006 | 11(45.8) | 10(13) | 0.001 |
Image/graph:
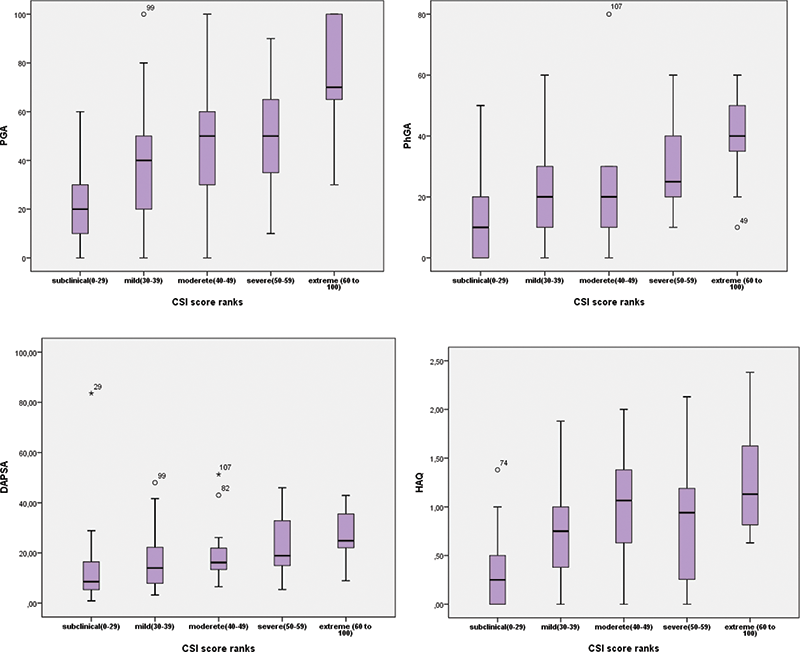
Figure 1. The positive correlation between PGA, PhGA, DAPSA, HAQ and CS severity in PsA patients
REFERENCES:
NIL.
Acknowledgements: NIL.
Disclosure of Interests None Declared.
Keywords: Fibromyalgia, Pain, Psoriatic arthritis
DOI: 10.1136/annrheumdis-2023-eular.6032