

Background EULAR guidelines advocate early detection and treatment of rheumatoid arthritis (RA) to induce a milder disease course. It was shown that early detection and treatment prevents erosive disease and maintains functional capabilities. Despite of that, the effect of early detection of RA on treatment related costs has never been investigated. Due to rising health care costs, it is important for society to keep health care affordable.
Objectives Our objective was to investigate whether early identification and treatment of RA patients (within 12 weeks after symptom onset) results in a reduction of treatment related costs when compared to a patient group that was seen after 12 weeks after symptom onset, stratified for ACPA status.
Methods Patients were obtained from the Leiden Early Arthritis Clinic (EAC), an inception cohort consisting of patients presenting with recent onset arthritis with a symptom duration ≤ 2 years. All consecutive RA patients fulfilling the 1987 and/or 2010 criteria, and who started a DMARD, included between May 2011 and December 2017 were evaluated, allowing a follow-up of 5 years. In this inclusion period, referral strategies were optimized for early recognition of RA. Early treatment start was defined as within 12 weeks after symptom onset. Information on medication use was obtained from prescription data from electronic patient records. Prices were used from both 2012 (at time of prescription) and 2022 (current). ACPA-positive and ACPA-negative RA were studied separately. Inverse probability weighting accounted for differences in patient characteristics between the early and late groups. The weighted average difference in medication costs was estimated with a generalized linear model with a log link and gamma distribution.
Results In total, 196 RA patients were ACPA-positive and 235 patients were ACPA-negative. Median (IQR) symptom duration was 5.5 (3-9) weeks in the early group, and 29.7 (19-53) weeks for the late group for ACPA-positive patients, and 6.4 (4-9) weeks and 26 (17-50) weeks in the ACPA-negative patients. At diagnosis, the early group of both ACPA-negative and ACPA-positive patients had more severe inflammation compared to the late group.
After 5 years, 6% of ACPA-negative patients and 20% of ACPA-positive patients had used ≥1 biological. The average number of biologics within these patients was 1 in the early ACPA-negative group, 1.4 in the ACPA-negative late group, and 1.9 and 2 in ACPA-positive early and late groups.
When using current price levels (2022), mean (sd) cost of treatment over 5 years was €11250 (25774) for ACPA-positive patients, and €3526 (11556) for ACPA-negative patients, while treatment costs among biological users was €44788 (36360) for ACPA-positive and 40896 (25123) for ACPA-negative RA.
After weighting, within ACPA-negative RA costs were lower in the early compared to the late group (€2877 versus €4213, respectively), β=1.46 (95%CI 0.32 – 3.4), indicating 46% higher costs in the late group. For ACPA-positive patients, costs were more similar (€11631 and €10988 respectively for the early and late group, β=0.96, 95%CI 0.52 – 1.8)(figure 1A). When 2012 prices were used, costs were in general higher: €14482 (29101) and €5158 (17897) for ACPA-positive and ACPA-negative patients, respectively. Comparing late and early groups using 2012 prices provided similar results in ACPA-negative RA (β=1.34 (95%CI 0.54 – 3.3), and a larger difference in costs for ACPA-positive RA (β=0.77 (95%CI 0.44 – 1.35)).
Conclusion Treatment-related costs of ACPA-positive RA are higher compared to ACPA-negative RA. However, early detection and treatment has the greatest impact on reducing treatment costs in ACPA-negative RA.
Image/graph:
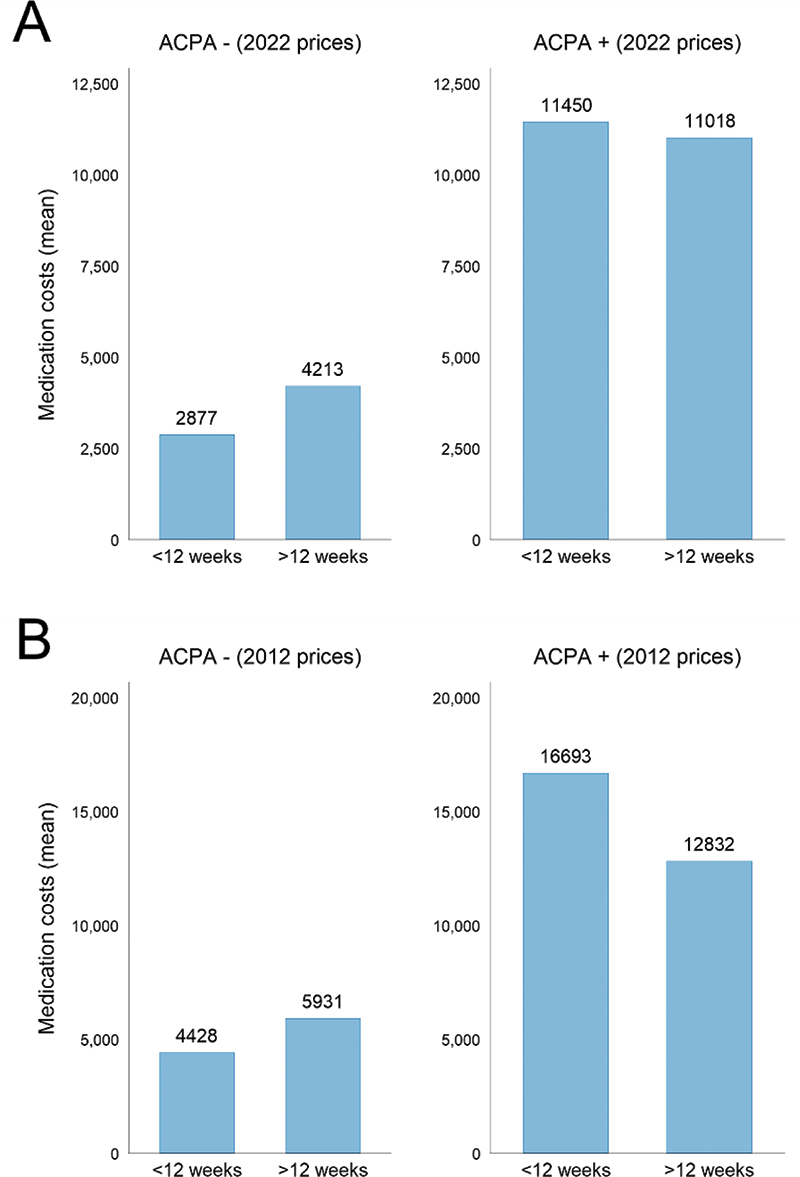
Figure 1. (A) Medication costs over 5 years indicated for ACPA-positive and ACPA-negative RA using current prices (2022), comparing early (<12 weeks after symptom onset) and later referral (>12 weeks after symptom onset). (B) Medication costs in euros over 5 years using prices at time of prescription (2012). ACPA: anti-citrullinated protein antibody
REFERENCES:
NIL.
Acknowledgements: NIL.
Disclosure of Interests None Declared.
Keywords: Epidemiology, bDMARD, Rheumatoid arthritis
DOI: 10.1136/annrheumdis-2023-eular.2021