

Background Patients with rheumatoid arthritis (RA) are at increased risk for serious infections (SI) and have a higher prevalence of multimorbidity. The increased risk for SI has led to the creation of multiple infection risk models over the last decade for patients with RA. These models often include combinations of patient demographics, medications, and a limited list of morbidities. However, the limited number of morbidities included in these models are not fully reflective of the morbidity burden seen in real-world practice. Thus, some morbidities that contribute to SI risk may be absent from the existing models.
Objectives We aim to examine associations between a comprehensive list of morbidities and SI in patients with RA.
Methods This population-based cohort study evaluated morbidities as risk factors for SI by including all adult patients from a geographically well-defined area from 1/1/1999 through 12/31/2013 who met the 1987 American College of Rheumatology criteria for RA. Patients were followed until the earlier of: death, migration from the region, or 12/31/2021. Fifty-five morbidities were evaluated as risk factors for SI and were ascertained from medical records using international classification of disease (ICD)-9 and ICD-10 codes, requiring 2 separate codes at least 30 days apart for inclusion. Serious infections were defined as infections requiring hospitalization and were identified using previously validated ICD-9 and ICD-10 codes where the primary diagnosis for hospitalization was infection. Conditional frailty models (a variation of Cox model that accounts for multiple events per patient) were used to analyze the association between each morbidity and SI. The first model adjusted for age, sex, and calendar year; the second model adjusted for age, sex, calendar year, and factors included in the Rheumatoid Arthritis Observation of Biologic Therapy (RABBIT) SI risk score;[1] the third model adjusted for age, sex, calendar year, and for factors included in the Mayo SI risk score.[2]
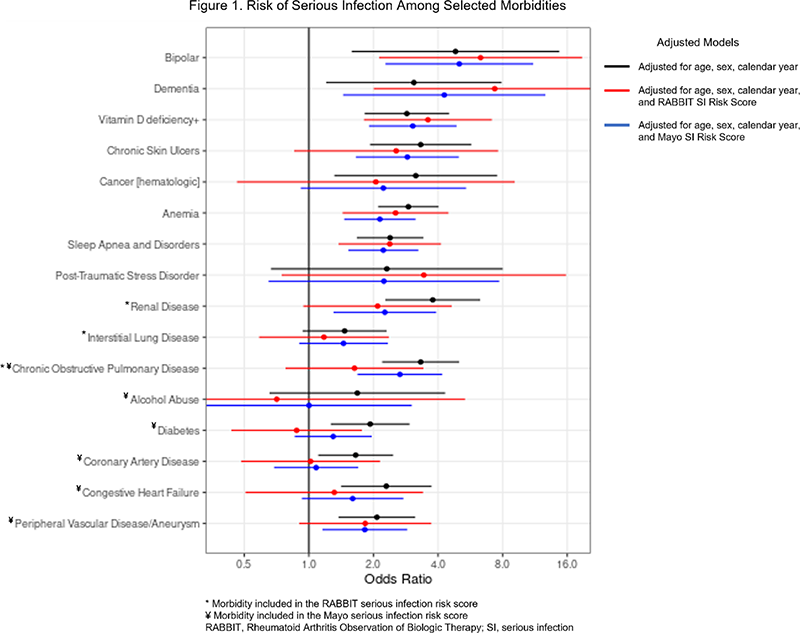
Results 911 patients (70% female, mean age 56 years, 66% seropositive) were included. The most common morbidities (% of patients; % person-years) included hypertension (53.6%; 40.9%), hyperlipidemia (54.6%; 37.4%), and osteoarthritis (55.2%; 32.6%). There were 293 SI among 155 patients (17%), which corresponded to an incidence of 3.9 SI per 100 person-years. Nineteen SI were fatal. Risk of SI was significantly increased in 26 of 55 morbidities in the initial model adjusted only for age, sex, and calendar year. In the RABBIT and Mayo SI risk score adjusted models, 12 and 23 morbidities were associated with increased risk, respectively. Morbidities conferring high risk among the three adjusted models are included Figure 1. Specific morbidities included in the RABBIT and Mayo SI risk scores continued to have large and/or significant effect sizes despite adjustment (Figure 1). The number of morbidities was also associated with SI risk, leading to a 16% (initial), 11% (RABBIT), and 13% (Mayo) increase in SI risk per morbidity.
Conclusion Several morbidities are associated with increased risk of SI in patients with RA, and this risk is not completely accounted for in two SI risk scores. Morbidity burden is an important clinical characteristic that may influence SI prevention strategies and treatment approaches in patients with RA.
References
Image/graph:
Acknowledgements: NIL.
Disclosure of Interests None Declared.
Keywords: Rheumatoid arthritis, Epidemiology
DOI: 10.1136/annrheumdis-2023-eular.875