

Background: Patients living with aPLs/APS are at increased risk of thrombosis and pregnancy morbidity. While aPLs/APS management remains controversial, little research exists regarding patient access to health information.
Objectives: The objective of this research is to understand the source, level of trust in, and perceived obstacles to accessing health information for patients with aPLs/APS.
Methods: Patients who had ≥1 positive aPL on ≥1 occasion or those who met the Revised Sapporo Criteria for APS were recruited from a Canadian APS clinic. Participants completed an online survey from 11/2022-04/2023 on the sources of health information they accessed and their trust in these sources at the time of diagnosis with aPLs/APS and within 6 months preceding survey completion. We calculated the percentage of patients accessing each source of information, quantified their trust in each source, identified perceived obstacles to accessing information and addressed whether they were negatively impacted by information from advocacy organizations, websites, or social media. McNemar tests were used to compare proportions of patients accessing and trusting information sources at time of diagnosis versus within the past 6 months.
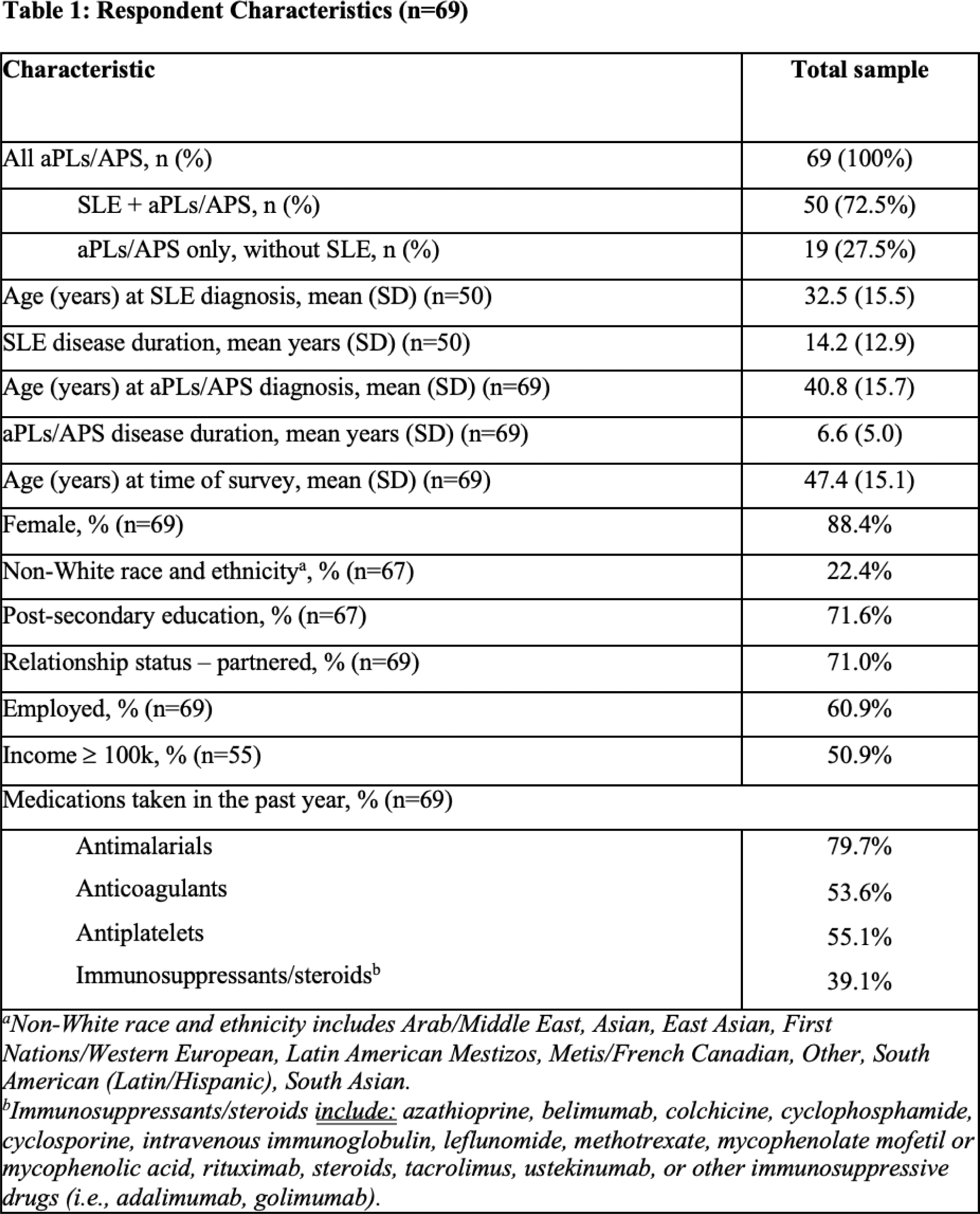
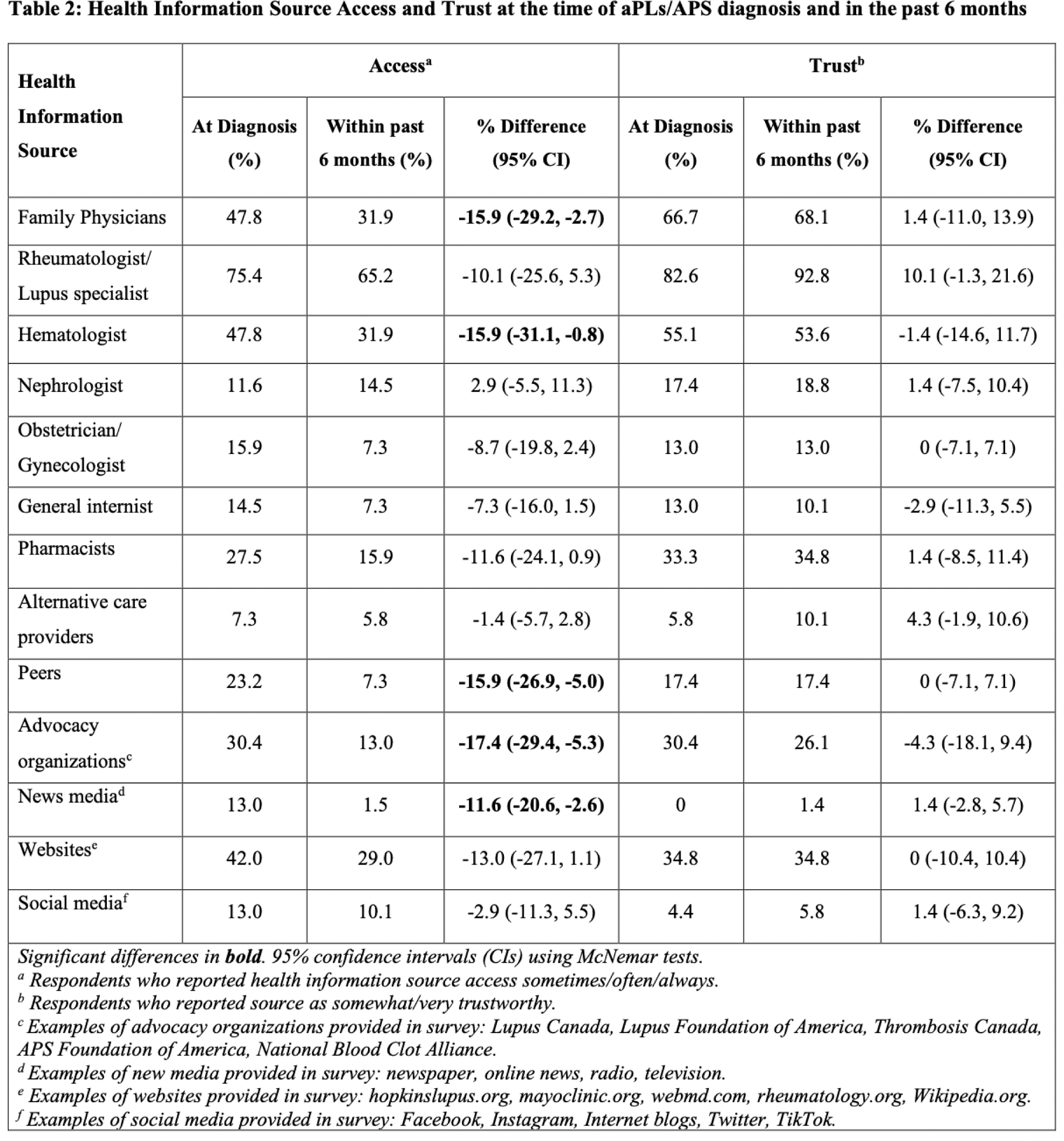
Results: 69 patients completed the survey (64% response rate); 88.4% were female, mean age at aPLs/APS diagnosis was 40.8 years (SD 15.7), 22.4% reported non-White race/ethnicity and 72.5% had aPLs/APS with SLE (per 1997 ACR or 2012 SLICC criteria) while 27.5% did not have underlying SLE (Table 1). The health information sources most frequently accessed both at diagnosis and in the past 6 months were rheumatologists/lupus specialists (75.4% vs. 65.2%), family physicians (47.8% vs. 31.9%) and hematologists (47.8% vs. 31.9%). The most trusted health information sources at diagnosis were rheumatologists/lupus specialists followed by family physicians and hematologists (82.6%, 66.7%, 55.1% respectively). At diagnosis, 42.0% of patients accessed websites (most commonly mayoclinic.org and hopkinslupus.org) and 13.0% accessed social media (most commonly Facebook and blogs). Only 30.4% of patients accessed and trusted advocacy organizations at diagnosis (Table 2). Challenges communicating with health care providers was the most frequently reported obstacle in accessing information related to aPLs/APS (20.3%). Of those who accessed the sources, some patients felt negatively impacted by information accessed through advocacy organizations (8.7%), websites (8.6%), and social media (9.1%).
Conclusion: Rheumatologists/lupus specialists, family physicians and hematologists were the most accessed and trusted sources of health information for patients both at aPL/APS diagnosis and within the past 6 months. However, 20.3% of patients felt communication with healthcare providers was an obstacle to accessing aPLs/APS information. Fewer than one third of patients accessed and trusted advocacy organizations and of those who accessed this source, some felt negatively impacted by the information found. There is a need for enhanced patient resources and outreach efforts through advocacy organizations as well as patient-physician communication pathways.
REFERENCES: NIL.
Acknowledgements: This study was funded by the M.S.I. Research Foundation. AEC holds The Arthritis Society Chair in Rheumatic Diseases at the University of Calgary.
Disclosure of Interests: Alexandra Kobza: None declared, Francesca Cardwell: None declared, Susan Elliott: None declared, Paul Gibson: None declared, Nancy Soliman: None declared, Leslie Skeith declares honoraria from Leo Pharma and Sanofi, and grant/research support from CSL Behring, Ann E. Clarke declares consulting fees from AstraZeneca, Bristol Myers Squibb, GSK, Otsuka, and Roche, and grant/research support from GSK, Megan Barber declares consulting fees from AbbVie, AstraZeneca, Janssen, GSK and Sanofi-Genzyme.