

Background: Antiphospholipid syndrome (APS) occurs when antiphospholipid antibodies (aPL) persist over time and cause arterial or venous thrombosis and/or pregnancy morbidity. Precise diagnosis is essential for optimal management of APS. Although the Sapporo classification criteria (1999) revised in Sydney in 2004 are widely acknowledged and used, they have been criticized for their inability to capture certain clinical manifestations of APS, apart from classic thrombotic and obstetric events. The ACR/EULAR criteria, which were recently developed in 2023, include additional clinical manifestations, like thrombocytopenia and livedo reticularis, which provide greater specificity while broadening the range of clinical features to be considered for diagnosis.
Objectives: To evaluate clinical applicability of ACR/EULAR 2023 criteria and distinguish its nuanced approach to APS diagnosis compared to Sydney criteria, regarding clinical and serological features included as new classification items.
Methods: Retrospective study of 81 patients with two separate positive determinations for antiphospholipid antibodies (aPL) at least 12 weeks apart at Hospital del Mar (Barcelona, Spain) between 2011 and 2021. Demographic, clinical, and biological data were collected. A bivariate statistical analysis was conducted in IBM® SPSS 25.0 using Chi-square or Fisher’s exact test for qualitative variables, and Student’s t-test or Mann-Whitney U test for continuous variables. Cohen’s kappa coefficient was calculated to assess agreement for APS classification between both criteria.
Results: Out of 81 patients, 62 (76.54%) were aPL asymptomatic carriers and 19 (23.46%) were classified as APS by either criteria set (Figure 1). Among them, 5 patients were classified as APS according to both criteria; 9 patients previously classified as APS with Sapporo criteria did not meet ACR/EULAR 2023 criteria anymore (mainly due to new definition of aPL titers), and 3 patients previously considered aPL-carriers were reclassified as APS using ACR/EULAR 2023. In total, 12 patients (14.8%) have been reclassified using ACR/EULAR 2023 criteria. Main clinical features that determined reclassification from aPL-carrier to APS were livedo reticularis and thrombocytopenia, being this association statistically significant (Table 1). No other significant associations were found. Sensitivity and specificity of ACR/EULAR 2023 in our cohort were 52.64% and 91.94%, respectively. We found moderate agreement between both diagnostic criteria with a _ of 0.481.
Conclusion: The ACR/EULAR 2023 criteria offer improved specificity for APS diagnosis, especially for cases without typical features. The incorporation of thrombocytopenia and livedo reticularis as distinct clinical criteria, as well as assigning different weights to aPL titers to heighten their varying thrombotic risk, poses an advantage for better APS classification and treatment in clinical practice. This may be especially true for males and women with no gestational history in whom the component derived from obstetric events is absent. Further research is still required to refine and validate classificatory criteria, balancing sensitivity and specificity, to achieve the best therapeutic approach.
REFERENCES: [1] Barbhaiya, Medha, et al. “The 2023 ACR/EULAR antiphospholipid syndrome classification criteria.” Arthritis & Rheumatology 75.10 (2023): 1687-1702.
[2] Sciascia, Savino, et al. “Identifying phenotypes of patients with antiphospholipid antibodies: results from a cluster analysis in a large cohort of patients.” Rheumatology 60.3 (2021): 1106-1113.
Distributon of patients regarding APS classification using both classification criteria
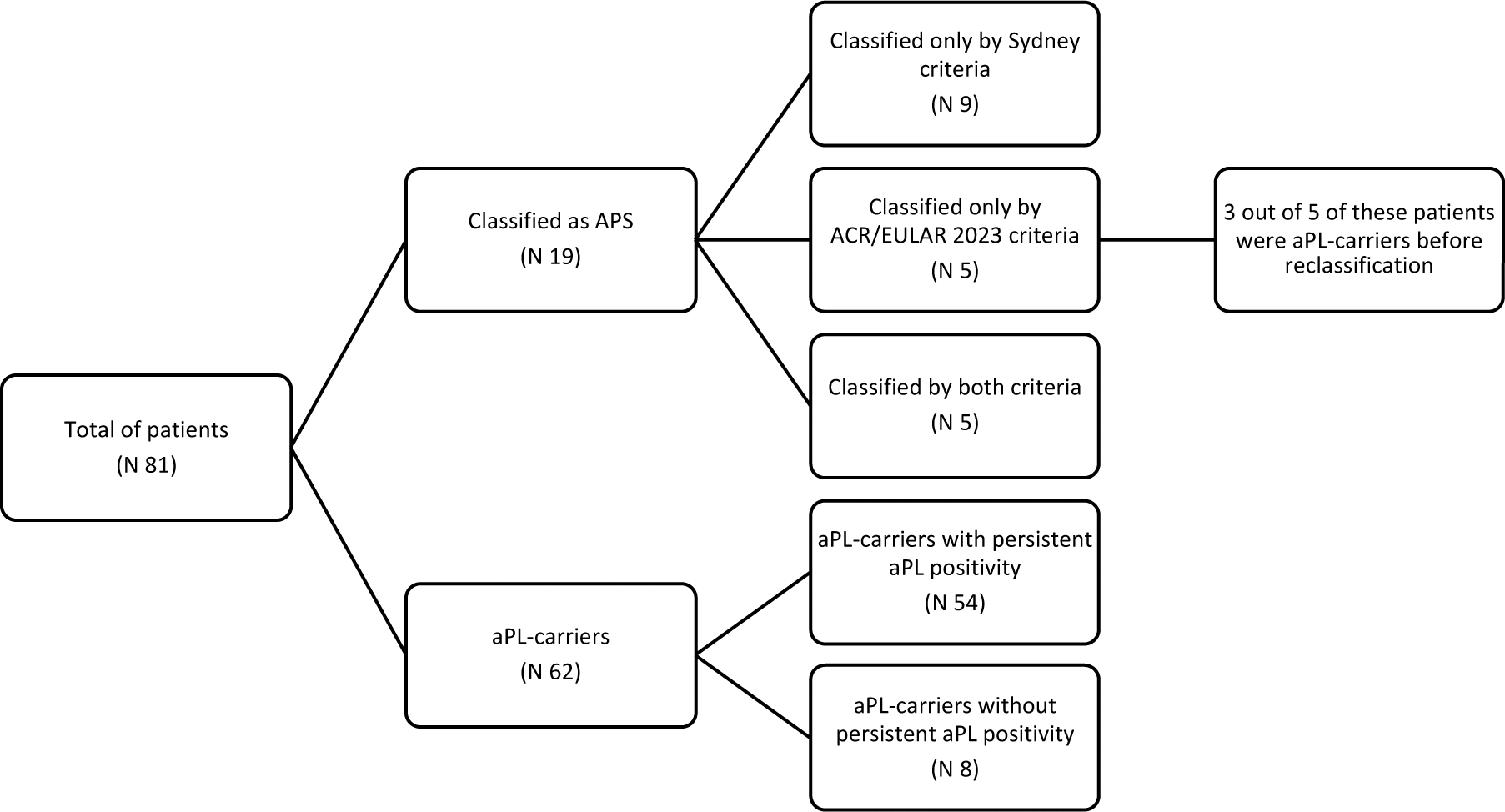
Table 1. Patients previously considered aPL-carriers, reclassified as APS using ACR/EULAR 2023
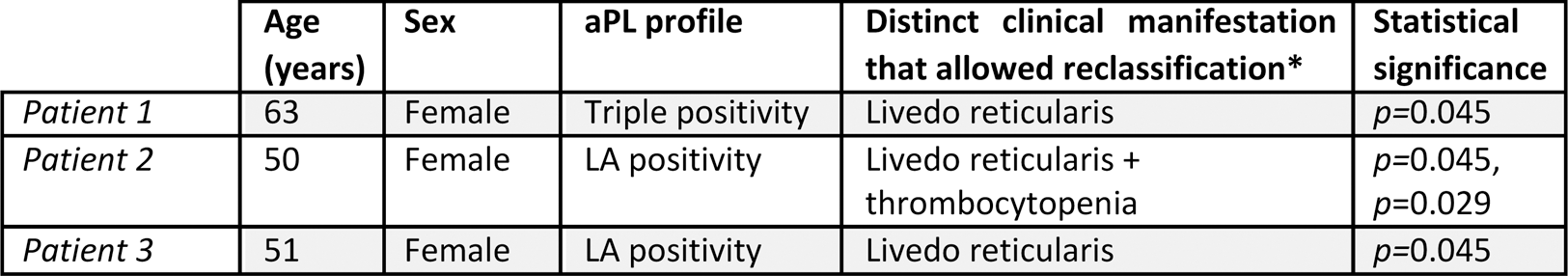
LA: lupic anticoagulant, aPL: antiphospholipid antibodies. * No treatment adjustments were necessary for any patient after reclassification.
Acknowledgements: NIL.
Disclosure of Interests: None declared.