

Background: It is known that triple positive antiphospholipid syndrome (APS-TP) is related to an increased presence of thrombotic and obstetric manifestations. Triple positivity is referred by the concurrence of anticardiolipin antibodies, anti-beta2 glycoprotein I antibodies and lupus anticoagulant. Up until the definition of the new American College of Rheumatology (ACR)/ European Alliance of Associations for Rheumatology (EULAR) classification criteria, APS was only classified by a laboratory domain and a clinical domain including thrombotic or obstetric events. The addition of other clinical manifestations called “non-criteria” will allow a greater number of patients to be early and systematically detected.
Objectives: To determine the prevalence of the new clinical manifestations included in the 2023 ACR/EULAR classification for APS-TP patients. To analyze the prevalence of “non-criteria” manifestations in the absence of thrombotic or obstetric events in patients with APS-TP.
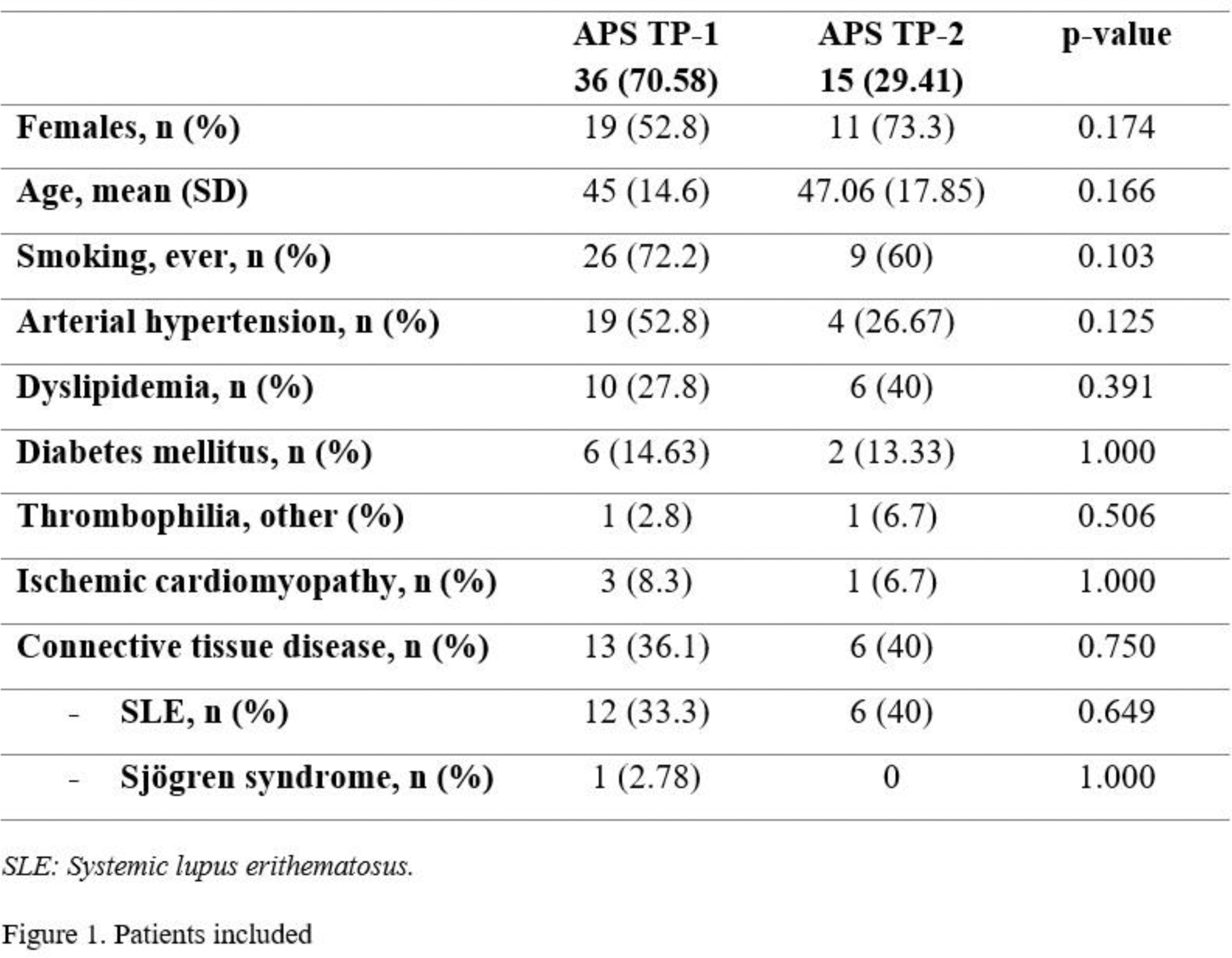
Methods: Cross-sectional descriptive study was carried out in a tertiary care hospital. APS-TP patients diagnosed between 1990 and 2023 were included. Patients under 18 years of age were excluded. Patients were classified into two groups: APS-TP with the presence of thrombotic and/or obstetric events (APS-TP1) and APS-TP with neither thrombotic nor obstetric events but with the presence of a non-criteria manifestation (APS-TP2). Sociodemographic, clinical and analytical variables were collected from both groups.
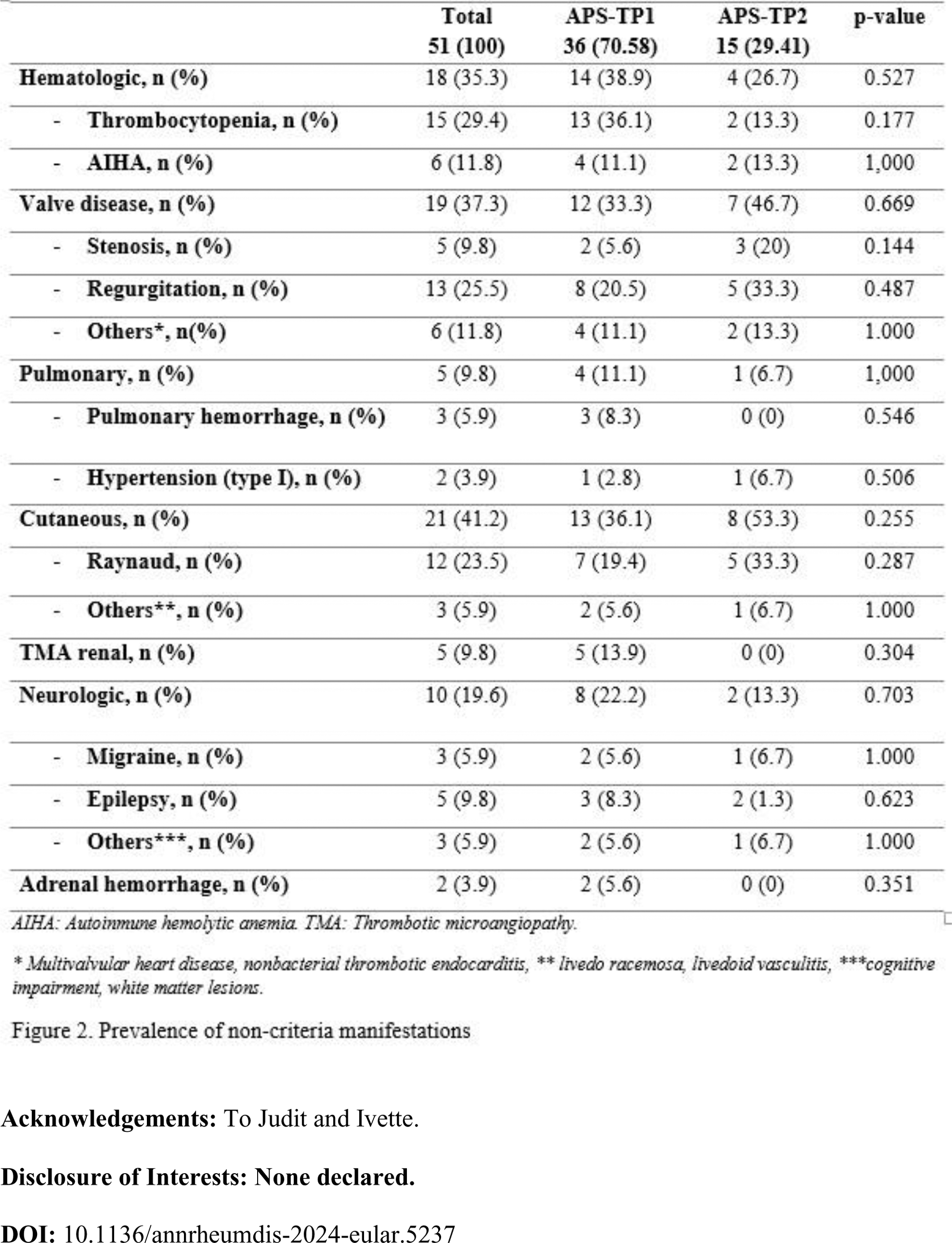
Results: A total of 51 APS-TP patients were identified, 36 (70.6%) APS-TP1 patients and 15 (29.4%) APS-TP2 patients. The majority of patients were female (59.3%) with a mean age of diagnosis of 47.2 years (Figure 1). Only 5 patients (9.8%) were classified as catastrophic APS. In the APS-TP1 group, 34 patients (66.7%) presented thrombosis (venous: 20 [58.8%], arterial 12 [35.2%] and both 4 [11.8%]) and 7 patients (13.7%) presented obstetric events. The most frequent ‘non-criteria’ manifestation in the APS-TP1 group was thrombocytopenia (36.1%), while in the APS-TP2 group was valvular heart disease (46.1%) followed by Raynaud’s phenomenon (33.3%). There were no significant differences in any of the observed variables (Figure 2).
Conclusion: In our cohort, the most common clinical manifestation overall was thrombosis. In patients without either thrombosis or obstetric events, the most prevalent manifestations were valvular heart disease and Raynaud’s phenomenon. The importance of studying antiphospholipid syndrome in patients with non-thrombotic manifestations is rising, especially in patients who do not meet criteria for other connective tissue diseases. Although some manifestations were exclusive to the thrombotic or obstetric morbidity group (renal microangiopathy, alveolar hemorrhage, bilateral adrenal hemorrhage), we did not find significant differences. This may be influenced by the small sample size, so it could be considered as a further object of study.
REFERENCES: NIL.
Acknowledgements: To Judit and Ivette.
Disclosure of Interests: None declared.