

Background: Primary antiphospholipid syndrome (pAPS) is a rare systemic autoimmune disease characterized by arterial, venous, or microvascular thrombosis, pregnancy morbidity, or no thrombotic manifestations in patients with persistent antiphospholipid antibodies (aPL). Migraine headaches are one of the commonest complaints in pAPS patients. Evidence reports non-specific capillary abnormalities in Nailfold capillaroscopy (NVC) from pAPS patients, and few previous investigations had shown debated abnormalities of blood flow at NVC study in patients with migraine without APS.
Objectives: Aims of this prospective study involving pAPS patients were to evaluate NVC abnormalities and their potential correlations with headache-related disability.
Methods: We performed a prospective study including patients fulfilling the following inclusion criteria: 1.a defined diagnosis of pAPS according to 2023 ACR/EULAR APS classification criteria; 2. age>18 y.o.; 3. no other connective tissue disease; 4. clinical diagnosis of migraine, assessed by an expert Neurologist. All patients referred to APS Reference Center at Rheumatology Unit of Tor Vergata University (Rome, Italy). Patients underwent clinical and laboratory assessment, NVC, and migraine headache tests including HIT-6 and MIDAS questionnaires (assessing headache-related disability) and PSQI test evaluating sleep quality. A moderate-severe level of disability was defined as MIDAS score ≥11, HIT-6 score ≥50, while a PSQI score ≥5 indicated a poor sleep quality. We also included healthy controls (HC). Continuous variables were compared with T test, categorical variables by using Chi-square or Fisher’s exact test. Linear logistic regression analysis was used to evaluate the adjusted risk of headache disability related to NVC variables. P<0.05 values were significant.
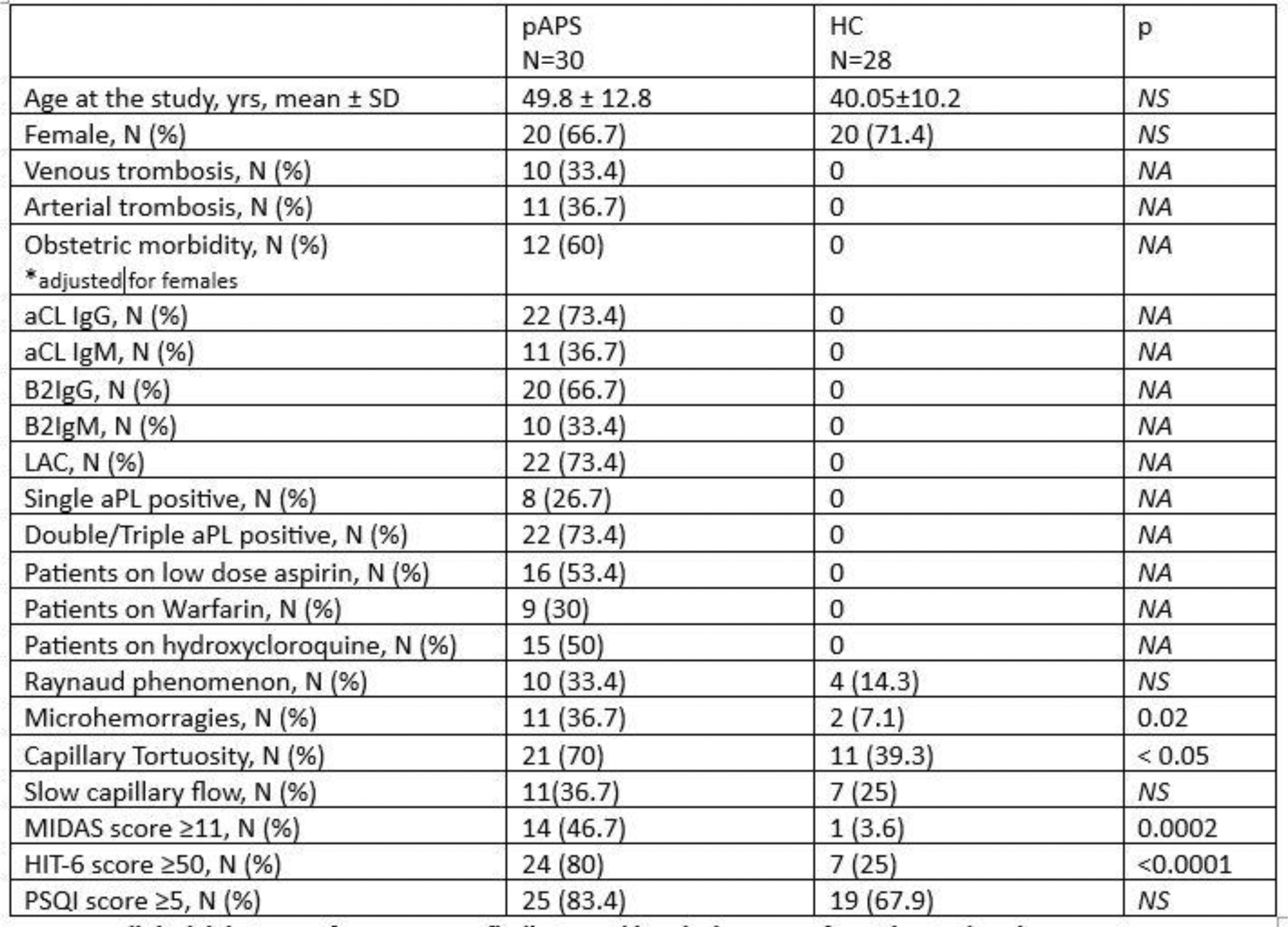
Results: The study cohort included 30 patients affected by pAPS and migraine, and 28 age and sex-matched HC Table 1). Thrombotic events as well as antiphospholipid antibodies (aPL) occurred only in pAPS group (Table 1). Raynaud phenomenon showed a trend to be more frequent in pAPS than in HC (Table 1). Patients with pAPS and migraine had microhemorrhages and tortuosity at NVC more frequently than HC (p=0.02 and p<0.05, respectively). Moreover, patients with pAPS showed a greater level of headache-related disability, as described by abnormal values of MIDAS and HIT-6 score than HC, while PSQI was similar between patients and HC (Table 1). Among pAPS patients, no differences in MIDAS, HIT-6, and PSQI scores occurred in accordance with the type of aPL positivity neither with the concomitant treatments (not shown). Linear logistic regression showed that a HIT-6 score ≥50 significantly correlated with slow capillary flow at NVC studies (OR 7.7, p= 0.03) in pAPS patients.
Conclusion: Headache-related disability could be relevant in pAPS patients in whom NVC abnormalities, mainly microhemorrhages and tortuosity, appear to be present in a higher percentage than in controls. Slow capillary flow, documented at NVC, might be strongly associated with headache-disability in pAPS patients.
Table 1. Clinical, laboratory features, NVC findings, and headache scores from the study cohort.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.