

Background: Gout is a chronic condition with a prevalence of up to 6.8%. Treatment with urate lowering therapy (ULT) is often under prescribed especially in primary care (PC), leading to frequent acute flares, requiring time off work and unnecessary hospitalisations. The “preventor to reliever ratio” in asthma has been previously shown to be a feasible quality index at a healthcare level, with reduction in asthma morbidity and mortality.[1]
Objectives: 1) To study the burden of disease, quality of care, and healthcare costs of gout using validated indices.
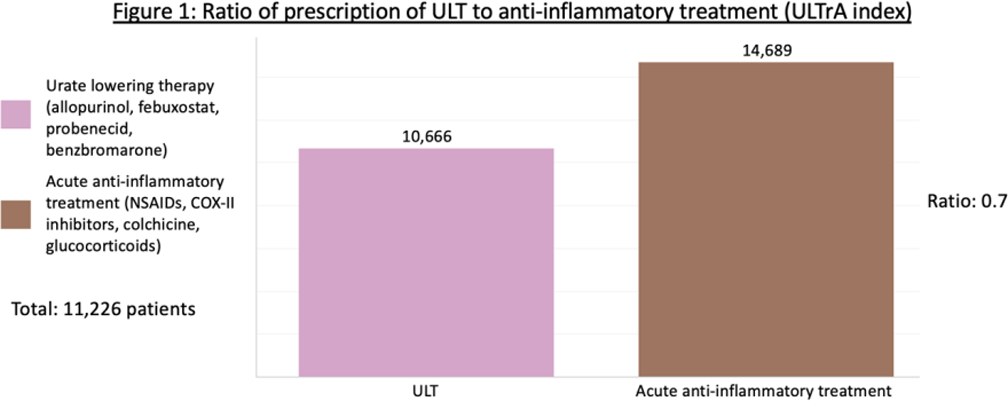
2) To propose a novel quality index – the “Urate Lowering Therapy to Acute Treatment ratio” (ULTrA), defined as the ratio of prescriptions for ULT to acute anti-inflammatory treatment for gout flares.
Methods: Retrospective study using data from electronic medical records of western Singapore, including 3 public acute hospitals and 7 PC clinics, from 1 January to 31 December 2022. We included patients aged 21 years and above with at least one gout-related healthcare encounter in any of the above institutions in the year 2022. The data was extracted from the National University Health System Value Driven Outcomes (VDO) database which integrates clinical, administrative and financial data, to visualise and study clinical quality indicators and cost of a defined cohort[2]. ETL (extract, transform and load) process was performed by VDO in-house tools and Microsoft SQL Server. Data analysis was performed using SQL and Tableau. Gout diagnosis was based on the International Classification of Diseases, 10 th Edition codes (M10, Y54.8, Z88.9, Z87.3, Z86.3 or T88.7). An Emergency Department encounter was defined by diagnosis of gout and prescription of acute anti-inflammatory treatment (nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine and/or glucocorticoids). An inpatient or outpatient encounter was included if gout was indicated as primary or secondary diagnosis.
Results: 11226 unique patients were included. Median age (IQR) 60.5 (40.5-80.5), 9341 (83.2%) male, 8242 (73.4%) Chinese, 1759 (15.8%) Malay and 507 (4.5%) Indian. 8976 (80%) were managed solely in PC.
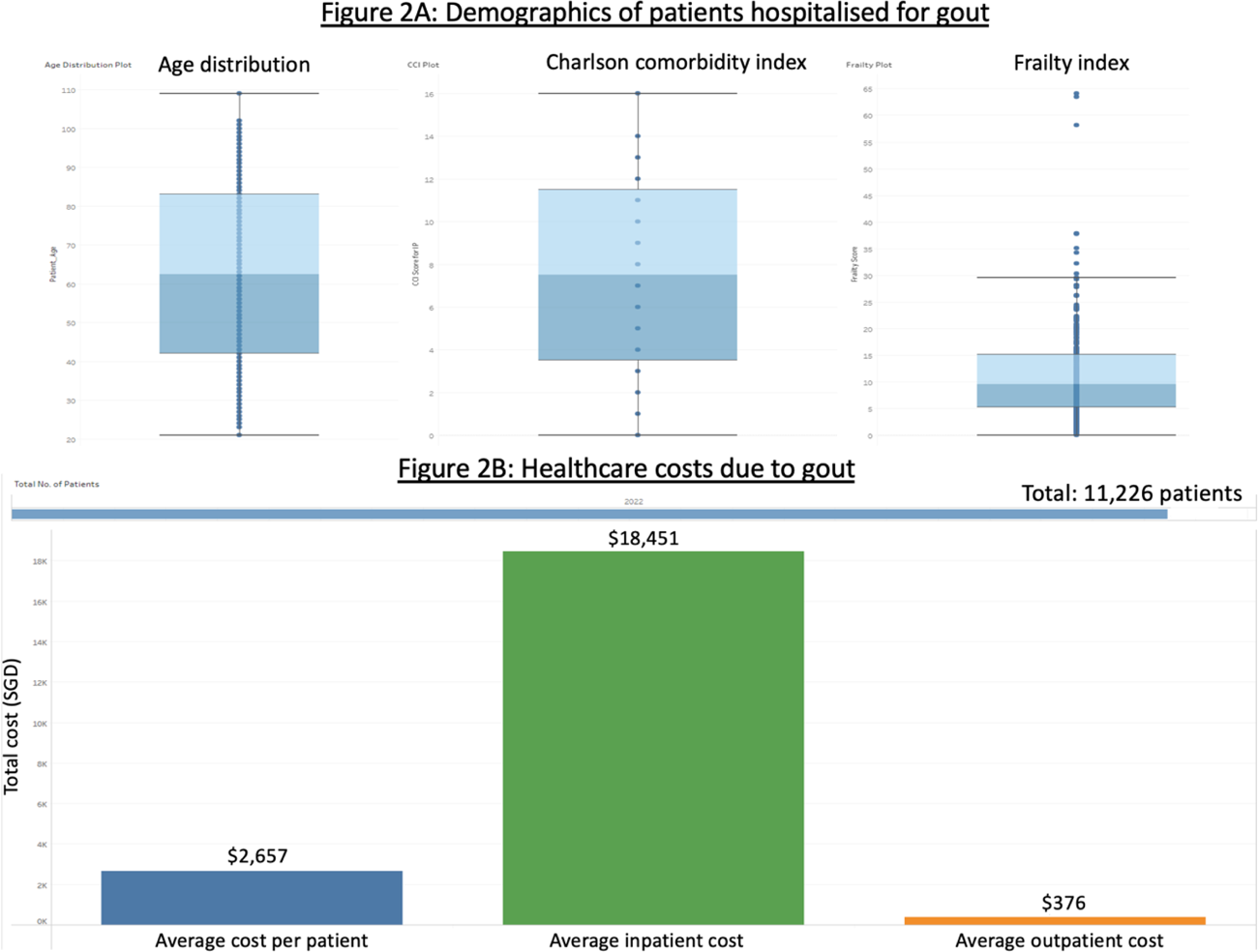
3028 (27%) had serum uric acid (sUA) measured at least twice in a year. Of 6576 patients who had sUA measured at least once, 2466 (37.5%) achieved target sUA of less than 360µmol/L at least once. 4888 (43.5%) had ULT prescriptions at least once (allopurinol, febuxostat, probenecid or benzbromarone). The ratio of prescriptions of ULT to acute anti-inflammatory treatment (ULTrA index) was 0.7 (Figure 1). 1381 (12.3%) required hospital admission with average hospital length of stay of 12.1 days. These patients were older, with median (IQR) age 62.5 (42-83) years, Charlson comorbidity index 7.5 (3.5-11.5) and frailty score 9.55 (5.2-50.1) (Figure 2A). Amongst patients of potential working age (21-60 years), 1967 (42.7%) received median (IQR) 32 (15.5-55.5) days off work due to gout. The annual cost of gout care, from the healthcare systems’ perspective, was SGD 2657 per patient, mainly driven by the patients requiring hospitalisation, with an inpatient annual cost of SGD 18451. For patients not requiring hospitalisation, annual cost was SGD 376 (Figure 2B).
Conclusion: Gout management is suboptimal leading to high rates of hospitalisation, time off work and healthcare costs. We propose monitoring and targeting a novel ULTrA index to improve overall gout management.
REFERENCES: [1] Chong, P. N., Tan, N. C., & Lim, T. K. (2008). Impact of the Singapore National Asthma Program (SNAP) on preventor-reliever prescription ratio in polyclinics. Annals of the Academy of Medicine, Singapore , 37 (2), 114–117.
[2] Lee, V. S., Kawamoto, K., Hess, R., Park, C., Young, J., Hunter, C., Johnson, S., Gulbransen, S., Pelt, C. E., Horton, D. J., Graves, K. K., Greene, T. H., Anzai, Y., & Pendleton, R. C. (2016). Implementation of a Value-Driven Outcomes Program to Identify High Variability in Clinical Costs and Outcomes and Association With Reduced Cost and Improved Quality. JAMA , 316 (10), 1061–1072.
Ratio of prescription of ULT to anti-inflammatory treatment (ULTrA index)
Demographics of patients hospitalised for gout; 2B: Healthcare costs due to gout
Acknowledgements: NIL.
Disclosure of Interests: May Shuen Tang: None declared, Sen Hee Tay: None declared, Shikha Kumari: None declared, Pamela Lim: None declared, Su Zin That: None declared, Htet Htet Aung: None declared, Peter Cheung Novartis, Novartis, Boehringer Ingelheim, AbbVie, Janssen, Manjari Lahiri Moderna (August 2023), AstraZeneca (October 2022), AbbVie (April 2022), J&J (March 2022), DKSH (August 2021), Conference sponsorship (EULAR 2022) by DKSH.