

Background: Osteoarthritis (OA) is the most prevalent joint disorder worldwide. Currently, the main management goal for OA is to control pain using adjunctive analgesic medications such as paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), and opioids. However, numerous studies have reported the adverse effects of analgesic medications, especially their long-term use, on the gastrointestinal, cardiovascular, and renal systems. Several studies have reported that melatonin exhibits the potential for pain relief and long-term safety profile. To date, no study has evaluated the effect of melatonin use on pain from OA and its potential mechanism.
Objectives: To examine the analgesic effects of oral melatonin on OA and investigate the underlying mechanism.
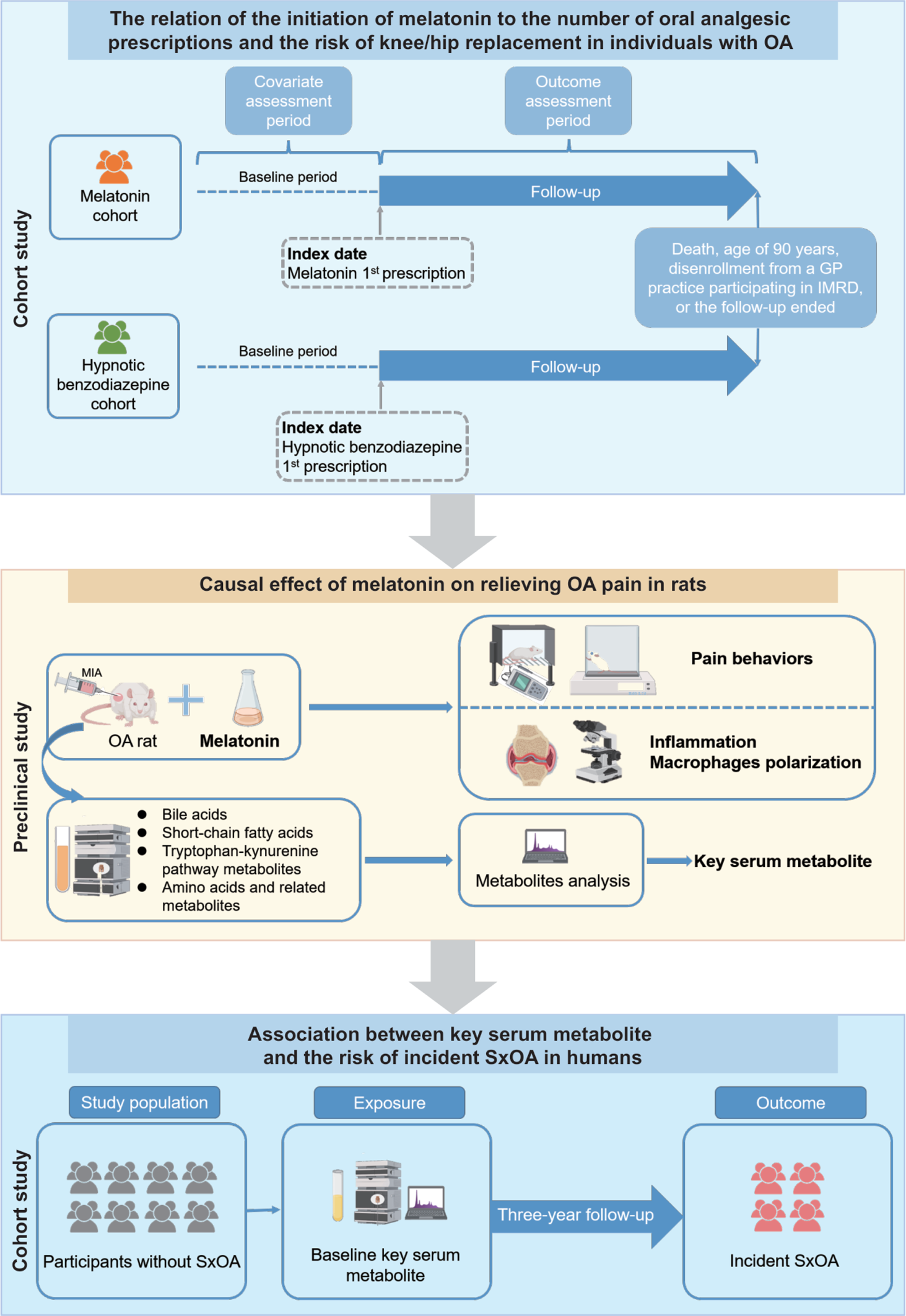
Methods: Using the United Kingdom primary care database (i.e., IQVIA Medical Research Database), we conducted a cohort study in individuals with OA to compare the number of oral analgesic prescriptions and the risk of knee/hip replacement between melatonin initiators and hypnotic benzodiazepines (i.e., active comparator) initiators using quantile regression models and Cox-proportional hazard models, respectively. To elucidate causation, we assessed the effects of melatonin on pain behaviors and explored several metabolites that may serve as potential regulatory agents of melatonin in the monoiodoacetate rat model of OA. Using data from another community-based cohort study, i.e., the Xiangya OA (XO) Study, we verified the relation of the key serum metabolite identified in the rat OA model, i.e., serum glycine, to the risk of symptomatic knee OA. Figure 1 shows a schematic illustration of this multi-component study.
Results: Compared with the initiators of hypnotic benzodiazepines (n=8,135), the melatonin initiators (n=813) had significantly fewer subsequent prescriptions of oral analgesics (50th percentile: 5 vs. 7, 75th percentile: 19 vs. 29, and 99th percentile: 140 vs. 162) and experienced a lower risk of knee/hip replacement (hazard ratio=0.47, 95%Cl: 0.30 to 0.73) during the follow-up period. Compared with vehicle control, rats treated with oral melatonin (20 mg/kg) had increased paw withdrawal thresholds (mean±SE: 63.43±3.66 g vs. 46.34±0.74 g) and weight-bearing asymmetry (mean±SE: 43.94±0.66 % vs. 34.16±2.28 %) at the terminal time point (P>0.99, P=0.44, respectively). Moreover, serum levels of glycine from rats treated with oral melatonin (20 mg/kg) were higher than those treated with vehicle control (mean±SE: 29,142±2186 nM vs. 17914±3594 nM). Using data from the XO Study (n=760), we observed an inverse association between baseline serum glycine levels and the risk of incident symptomatic knee OA during a 3-year follow-up. For one standard deviation increase in the level of serum glycine, the crude OR of SxOA was 0.87 (95% CI: 0.67-1.12, P=0.27), and the multivariable-adjusted OR was 0.71 (95% CI: 0.51-0.99, P=0.04).
Conclusion: In conclusion, this general population-based cohort study presents the first evidence suggesting that melatonin therapy reduces the number of prescriptions of analgesic medications and lowers the risk of joint replacement surgery in people with OA. Glycine may play a role in the effect of melatonin on pain from OA. Given its safety profile, melatonin may be a potential agent for treating chronic pain from OA, and future randomized controlled trials are warranted.
The schematic illustration of this study. OA, osteoarthritis; GP; general practitioners; IMRD, IQVIA Medical Research Database; MIA, monoiodoacetate; SxOA, symptomatic knee osteoarthritis.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.