

Background: Psoriatic arthritis (PsA) is a persistent inflammatory condition affecting both the skin and joints, and individuals with this condition face a heightened risk of cardiovascular disease, which remains a primary cause of mortality in this group. The increased cardiovascular risk has been associated with disease characteristics that induce a systemic inflammatory state resulting in atherosclerosis development and endothelial damage. Various cardiovascular risk assessment algorithms are employed to evaluate the risk in this population, with the 2013 American College of Cardiology/American Heart Association (ACC/AHA) algorithm being among the most widely used. Notably, in 2023, the AHA introduced the Predicting Risk of CV Disease EVENTs (PREVENT TM ) algorithm as an updated tool for evaluating the 10-year risk of developing atherosclerotic cardiovascular disease.
Objectives: We aimed to assess the effectiveness of the 2013 ACC/AHA and the 2023 PREVENT TM algorithms to detect the presence of carotid plaque (CP) and to evaluate the cardiovascular risk reclassification with the carotid ultrasound in PsA patients.
Methods: This was a cross-sectional study. We recruited a total of 101 patients with PsA diagnosis, according to the 2006 CASPAR classification criteria, aged 40-75 years. Patients with a previous cardiovascular event were excluded. Cardiovascular risk was evaluated with the 2013 ACC/AHA and the 2023 PREVENT TM algorithms. A carotid ultrasound was performed to all study subjects by a certified radiologist blinded to clinical information. The presence of CP was considered as a carotid intima media thickness ≥ 1.2 mm or a focal narrowing ≥ 0.5 mm. Distribution was evaluated with the Kolmogorov-Smirnov test. Correlations were performed with the Spearman-rho coefficient (rho). A ROC-curve analysis was performed for both algorithms. A p-value < 0.05 was considered statistically significant.
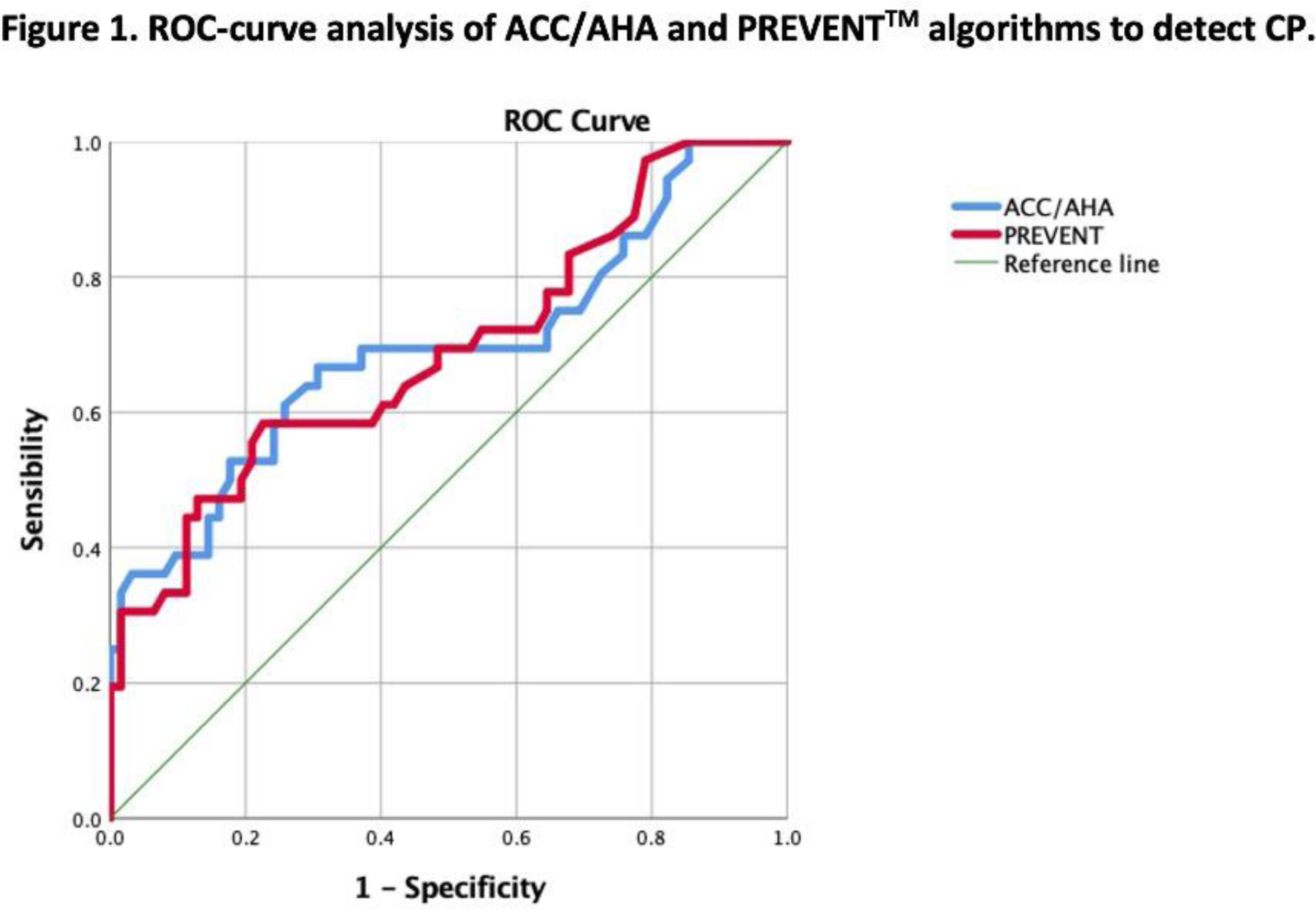
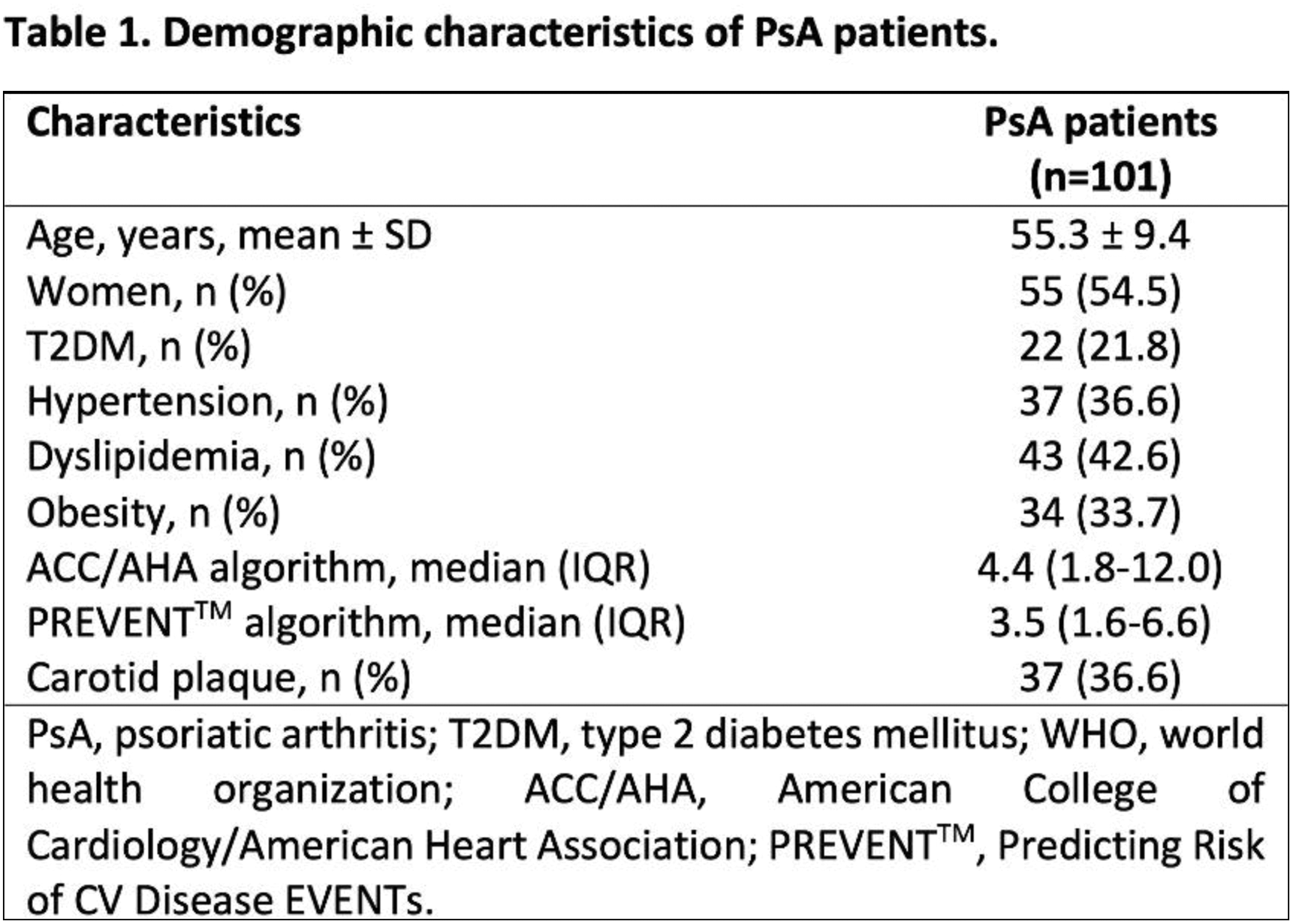
Results: The presence of CP was detected in 37 (36.6%) patients. Demographic characteristics are shown in Table 1. There was a large positive correlation between the PREVENT TM and the ACC/AHA algorithms (rho = 0.864, p = <0.001). Both algorithms showed significant discrimination for the presence of CP in PsA patients, the PREVENT TM algorithm had an AUC 0.691 (95% CI 0.579-0.804, p = 0.002), with a cutoff point of 3.55, sensibility of 61.1% and specificity of 58.1%. The ACC/AHA algorithm had an AUC 0.694 (95% CI 0.579-0.810, p = 0.001) with a cutoff point of 4.75, sensibility of 66.7% and specificity of 62.9% (Figure 1). Following carotid ultrasound, 34 patients (33.7%), initially categorized as low, borderline, or intermediate risk using the PREVENT TM , were subsequently reclassified to high cardiovascular risk due to the identification of CP. Furthermore, 25 (24.8%) patients, initially classified as low or intermediate risk with the ACC/AHA algorithm, were reclassified to high cardiovascular risk.
Conclusion: Our findings indicate that both algorithms exhibited significant discrimination for the presence of CP. Nevertheless, the identified cutoff points for CP, as determined by both algorithms, fall within the category of low cardiovascular risk. Notably, a substantial number of patients were reclassified to high cardiovascular risk following carotid ultrasound, particularly with the PREVENT TM algorithm. The incorporation of the carotid ultrasound as part of the cardiovascular assessment in PsA patients should be considered, as the algorithms appear to underestimate the actual cardiovascular risk in this population.
REFERENCES: NIL.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.