

Background: Biologic therapy has been linked to lipid alterations without changes in cardiovascular disease outcomes. The effect of biologic therapy on lipid parameters among psoriatic arthritis (PsA) patients treated with biologic Disease-Modifying anti-rheumatic drugs (bDMARDs) has not been defined.
Objectives: To compare serum lipid levels, cardiovascular risk, the prevalence of carotid plaque (CP), and increased carotid intima-media thickness (cIMT) between PsA patients with and without biologic treatment.
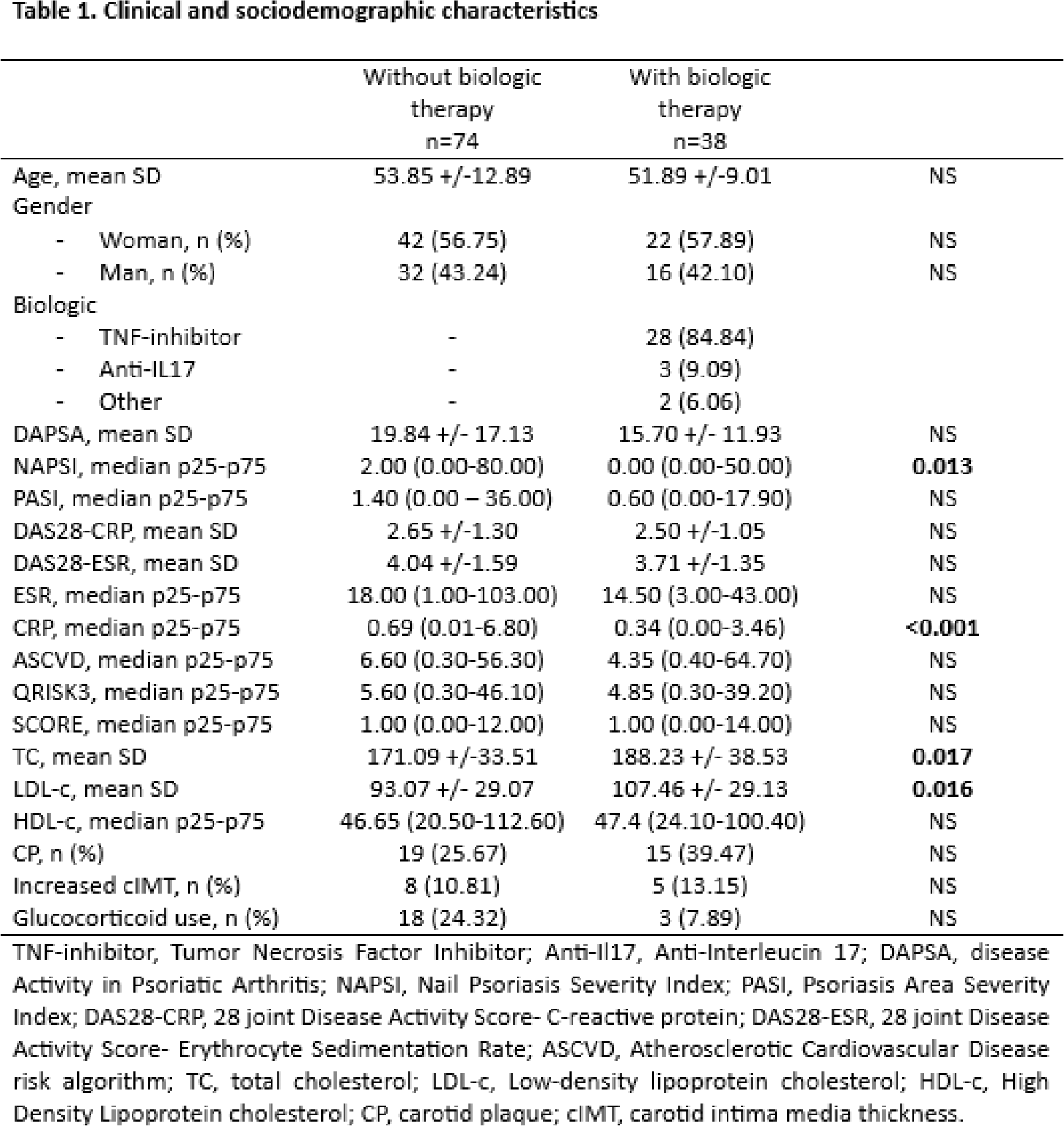
Methods: We performed an observational, comparative, and cross-sectional study in patients who fulfilled the 2006 Classification Criteria for Psoriatic Arthritis (CASPAR). Patients with a history of previous atherosclerotic cardiovascular disease and pregnancy were excluded. Disease activity was measured using the Disease Activity for Psoriatic Arthritis Score (DAPSA), Psoriasis Severity Index (PASI), and Nail Psoriasis Severity Index (NAPSI). Cardiovascular risk was estimated with ASCVD, QRISK3, and SCORE calculators. Carotid B-mode ultrasonography was employed to measure carotid intima-media thickness (cIMT) and detect carotid plaques (CP). Descriptive analysis included frequencies (%), mean (± SD), and median (p25-p75), and comparisons with Chi-square, Student ́s t, and Mann-Whitney U test. We considered p<0.05 significant.
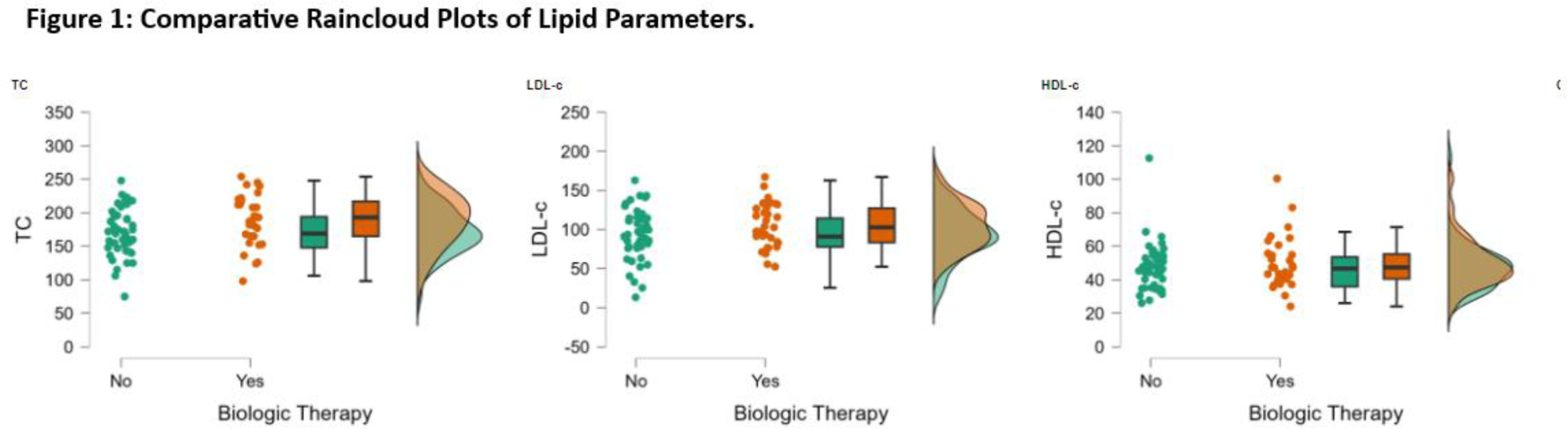
Results: We recruited 112 patients who fulfilled the criteria. The prevalence of bDMARD use was 33.92%. The most frequent bDMARDs used were TNF inhibitors (84,84%). Patients in biologic therapy had a significantly lower NAPSI score than those with synthetic DMARDs [0.00 (0.00-50.00) vs. 2.00 (0.00-80.00), p =0.013]. We found no significant differences in DAPSA, PASI, DAS28-CRP, or DAS28-ESR. Patients with biologic therapy had higher total cholesterol (TC) [188.23 ±38.53 vs. 171.09 ± 33.51; p=0.017] and Low-Density Lipoprotein cholesterol (LDL-c) [107.46 ± 29.13 vs. 93.07 ±29.07; p=0.016] than those without biologic therapy. No significant differences were found between biologic therapy and cardiovascular risk, CP prevalence, or between biologic therapy and prevalence of increased cIMT. (Table 1, Figure 1)
Conclusion: In this population, patients treated with bDMARDs had higher levels of CT and LDL-C, without significant differences detected in cardiovascular risk, prevalence of CP, or increased cIMT. However, prolonged exposure to increased levels of LDL-C and TC is associated with a higher cardiovascular risk. Close monitoring and early intervention of lipid levels in patients treated with biological therapy is imperative.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.