

Background: Rheumatoid arthritis (RA) is a chronic inflammatory disease that can transit to multiple progressive articular and extra-articular damage if left untreated. Short-chain fatty acids (SCFAs) have shown to be associated with onset of arthritis. We hypothesized that SCFAs may associate with polyarthritis (joint swelling) and interstitial lung disease (ILD) that have not been studied.
Objectives: To explore the relationship between SCFAs and progression of RA.
Methods: We measured the serum SCFA levels in 282 established RA patients undergoing standard treatment though high performance liquid chromatography coupled to a tandem mass spectrometer (HPLC-MS/MS) methodologies. Among these patients, 205 were RA with musculo-skeletal pain and no joint deformity, including 91 with positive for anti-citrullinated protein antibodies (ACPA+RA) and 114 with negative for ACPA (ACPA-RA). In addition, of all 282 established RA patients, 40 individuals had ILD (RA-ILD).
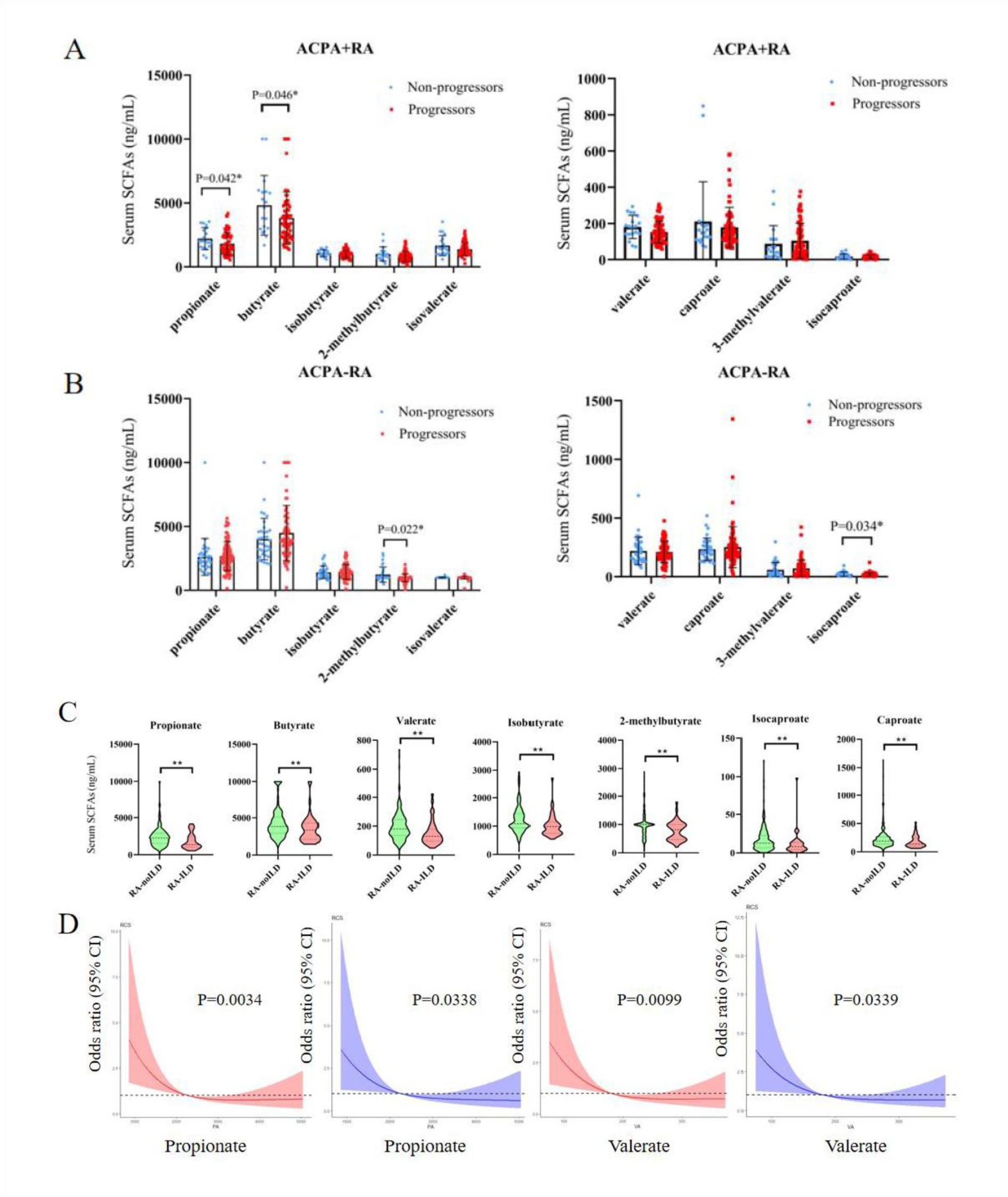
Results: In ACPA+RA patients, butyrate and propionate in patients progressed to polyarthritis (joint swelling) were significantly reduced compared to individuals not progressed to joint swelling. However, this was not the case in ACPA-RA patients, propionate and butyrate were not associated with the progression of polyarthritis. These findings suggested that SCFAs can affect the risk of RA progression to multiple arthritis, especially in ACPA+RA patients. In addition, serum SCFAs of RA-ILD patients was significantly lower than that of RA-nonILD. Univariate and multivariable logistic regression analysis demonstrated that lower levels of propionate and valerate were significantly correlated with the occurrence of ILD. Further, we found both propionate and valerate were negatively associated with risk of ILD in a nonlinear manner by using the restricted cubic spline nested in logistic regression. The decrease in propionate below 2179 ng/mL and valerate below 172 ng/mL was associated with a rapid increase in the risk of ILD both in univariable and multivariable analyses.
Conclusion: We first showed that mean SCFA levels in patients with polyarthritis and RA-ILD were significantly reduced, suggesting that lower SCFAs at a certain level increase the risk of polyarthritis and ILD. SCFAs significantly reduce inflammation, regulate the immune response of intestinal tract and other distal mucosal sites, and delay the clinical progress of RA. Therefore, increasing the level of SCFAs through dietary and restoring immune balance supplement is a potential therapeutic strategy to slow down the progress of RA and reduce mortality.
REFERENCES: [1] Tajik N, Frech M, Schulz O, et al. Targeting zonulin and intestinal epithelial barrier function to prevent onset of arthritis. Nat Commun 2020;11:1995.
[2] Martinsson K, Dürholz K, Schett G, et al. Higher serum levels of short-chain fatty acids are associated with non-progression to arthritis in individuals at increased risk of RA. Ann Rheum Dis 2022;81(3):445-7.
[3] He J, Chu Y, Li J, et al. Intestinal butyrate-metabolizing species contribute to autoantibody production and bone erosion in rheumatoid arthritis. Sci Adv 2022;8(6):eabm1511.
[4] Ashique S, De Rubis G, Sirohi E, et al. Short Chain Fatty Acids: Fundamental mediators of the gut-lung axis and their involvement in pulmonary diseases. Chem Biol Interact 2022;368:110231.
Serum level distribution of SCFAs in RA patients. (A) The levels of SCFA in ACPA+RA progressed and not progressed to polyarthritis (joint swelling); (B) The levels of SCFA in ACPA-RA progressed and not progressed to polyarthritis (joint swelling); (C) Difference of serum SCFAs between RA-ILD and RA-nonILD by Mann-Whitney U test; (D) Odds ratio curves of propionate and valerate by using the restricted cubic spline (RCS) for ILD in the RA patients. The red curve was derived from univariable analysis, and the blue curve derived from multivariable analysis after adjusting gender, age, duration of diabetes, BMI, smoking, ESR and CRP levels.
Acknowledgements: NIL.
Disclosure of Interests: None declared.