

Background: Rheumatoid arthritis (RA) is a chronic, inflammatory, autoimmune disease. Abnormalities in T-cell subset frequencies have previously demonstrated (1,2) their utility in predicting progression from the at-risk stage, as well as response to methotrexate (MTX) in early RA and flare when in remission (2-5). However, the value of baseline T-cell subsets for predicting response to anti-TNF has not been evaluated.
Objectives: The aim of this study was to assess the value of T-cell subsets for predicting response to anti-TNF in patients with RA, and observe changes in T-cell subtypes over time on MTX or anti-TNF treatment.
Methods: RA patients (ACR/EULAR 2010 classification) were recruited from the Leeds early RA clinic. Patients were managed using NICE guidelines for the MTX. Anti-TNF treatment was part of clinical trials of early intervention (VEDERA/EMPIRE). DAS28(CRP)-remission was used to classify response. Patients not in remission continued treatment when on anti-TNF or received additional DMARDs (synthetic/biologic) when on MTX. T-cell subsets (naive CD4+ cells, T-regulatory cells (Treg) and inflammation related cell (IRC) were measured by flow-cytometry by NHS-services. Baseline data are described using medians and proportion. Predicting of the achievement of remission at 6 months was performed using forward binary logistic regression. Repeated measures over time were analysed using two-way mixed ANOVA test.
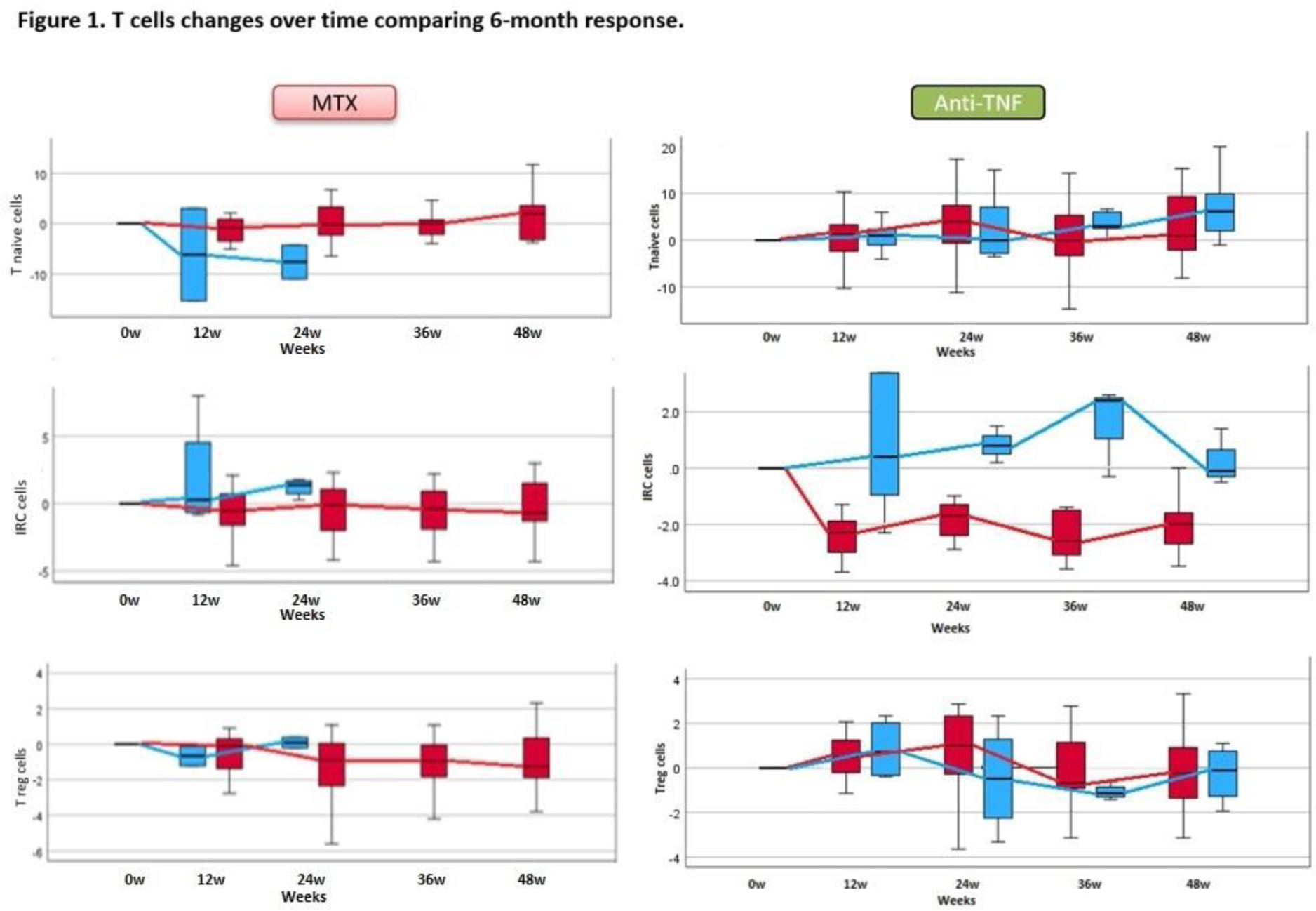
Results: 221 patients were treated with MTX and 78 patients with anti-TNF. At 6m in the MTX group 50.7 % patients achieved remission versus 61.5% for anti-TNF. In the MTX-group, baseline TJC, SJC and CRP were associated with remission (p<0.05) as well as naïve T-cell frequencies (p<0.0001). Modelling using clinical data only, suggested predictive value for remission for age, smoking and CRP (Accuracy=67.5%/AUC=0.731). Adding the T-cell subsets to the model, improved accuracy to 71.9%/AUROC=0.767. A similar analysis for anti-TNF induced remission suggested only a significant association with TJC (p=0.019) and weak association with Treg (p=0.253). Modelling did not retain any demographic/clinical parameters and adding T-cell subsets did not allow a model to be built. Over-time in the MTX group, there was a reduction in naïve T-cell frequency in non-responders (Figure 1, Blue, n=21) but not in patients achieving remission (n=13). IRC were stable in the remission but increased in the non-responder group. Treg reduced over time.
In the anti-TNF group, IRC reduced quickly in remission (n=25) but not in patients with active disease (n=5). There was no clear trend for increase/reduction in naïve cells in either group, and Treg remained relatively stable in both groups.
Conclusion: The added value of T-cell subsets for predicting MTX remission was clearly demonstrated by the improvement of accuracy/AUC compared to using clinical data alone, validating previous smaller studies (1,2). There are still no biomarkers of the response to anti-TNF in early RA. Anti-TNF prevented the loss of both Treg and naïve T-cells seen in MTX non-responders. Response to MTX but not anti-TNF, is predicted by T-cell subsets. This is consistent with the fact that anti-TNF is prescribed and works when MTX fails.
REFERENCES: [1] Ponchel F, et al. Blood. 2002;100(13):4550-4556.
[2] Gul HL, et al. Clin Exp Rheumatol. 2023;41(1):126-136.
[3] Ponchel F, et al. Ann Rheum Dis. 2014;73(11):2047-2053.
[4] Szalay B, et al. Clin Rheumatol. 2014;33(2):175-185.
[5] Saleem B, et al. Ann Rheum Dis. 2010;69(9):1636-1642.
Acknowledgements: NIL.
Disclosure of Interests: None declared.