

Background: Rheumatoid arthritis (RA) is a chronic, systemic, immune-mediated inflammatory disease that mainly targets the joints. The pathogenesis of RA involves dysregulations in immune pathways such as the JAK-STAT signaling pathway. JAK inhibitors (JAKi) are a class of disease modifying anti-rheumatic drugs that are approved for RA treatment.
Objectives: To compare the in-vitro cellular effect of two JAKi, tofacitinib and upadacitinib, in peripheral blood leukocytes from patients with untreated early rheumatoid arthritis (ERA), established refractory RA and healthy individuals.
Methods: Blood samples were collected and peripheral blood mononuclear cells (PBMCs) were isolated and cultured during 24 hours with either tofacitinib or upadacitinib. The frequency, phenotype, STAT phosphorylation levels (pSTAT) and apoptosis of B cells, T cells, monocytes and dendritic cells (DCs) were analysed by flow cytometry before and after cell culture with JAKi in all groups.
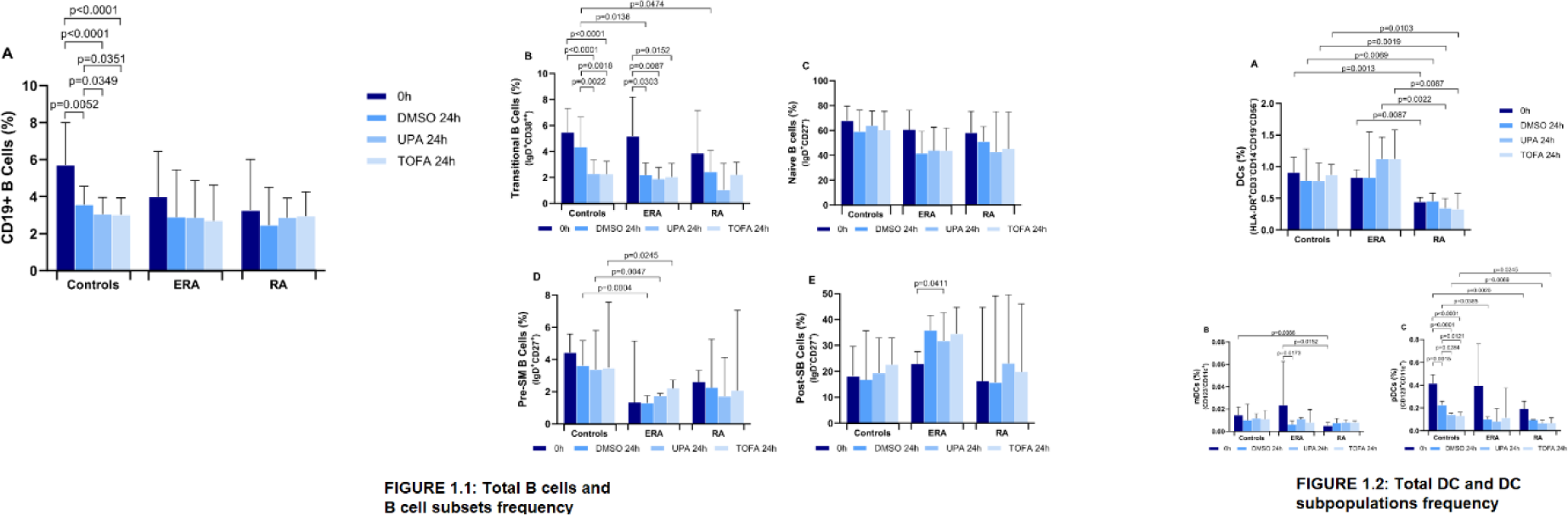
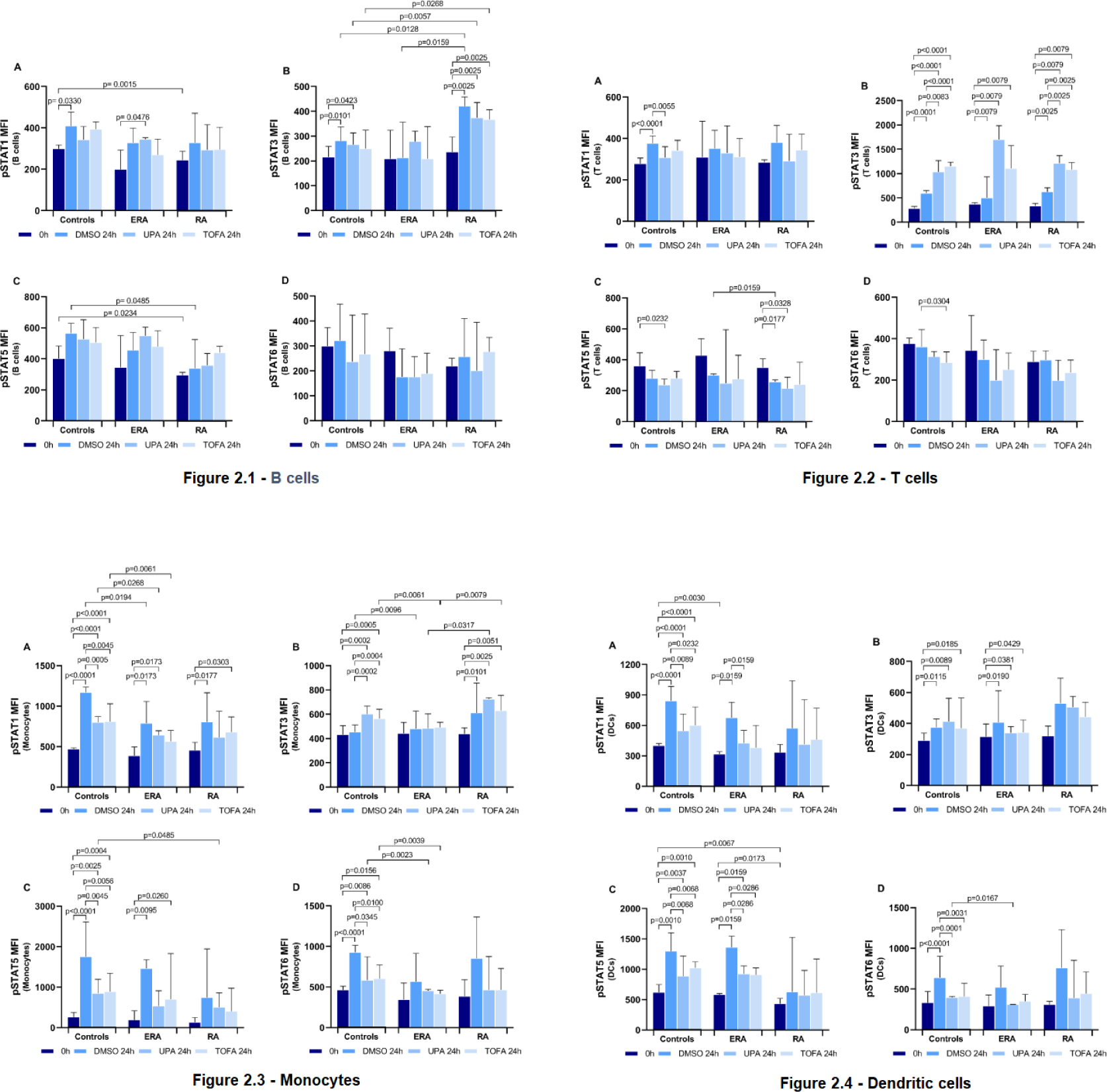
Results: We included 6 patients (50 % female, 55.0±22.1 years old, with a mean disease duration of 6.2 months). Changes in the frequency of B cells and DCs’ subpopulations, but not in T cells or monocytes, were observed after 24 hours of in vitro cell culture with both JAKi (Figure 1). Furthermore, phenotypic analysis has revealed a reduction in the expression of activation markers on B cells, T cells and monocytes after culture with upadacitinib and tofacitinib. In addition, changes in pSTAT levels measured by median fluorescence intensity (MFI) were also detected in all leukocyte populations after culture with both JAKi when compared to baseline and/or drug vehicle (Figure 2). Notably, JAKi did not significantly affect cell viability.
Conclusion: Overall, our data supports a similar immunomodulatory effect of tofacitinib and upadacitinib in peripheral blood leukocytes of early untreated RA.
The frequency of total CD19+ B cells and B cell subsets (1.1), and the total dendritic cells (DC) and DC subsets (1.2) after 24 hours of in vitro cell culture with upadacitinib and tofacitinib.
Changes in STAT phosphorylation levels in B cells (2.1), T cells (2.2), monocytes (2.3) and dendritic cells (2.4) after 24 hours of in vitro cell culture with upadacitinib and tofacitinib.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.