

Background: Patients with primary dry syndrome have a disturbed gut microbiota with metabolic dysfunction. The impact of gut microbiota on disease progression in patients with pSS is not yet fully understood, despite a growing body of research suggesting that a healthy gut microbiota is essential for patients with pSS.
Objectives: The aim of this study was to investigate the combined effects of gut microbial disorders on disease activity and immune function in patients with pSS and to screen possible biomarkers as potential biomarkers for predicting disease progression.
Methods: This study recruited 49 patients with pSS between November 2018 and September 2020 All pSS patients met the 2016 American College of Rheumatology (ACR)/European Alliance of Associations for Rheumatology (EULAR) joint revised classification and diagnostic criteria. All included cases were not taking systemic antibiotics and probiotics one month before each sample collection. Patients with severe infections, malignant tumors and other autoimmune diseases were excluded. Baseline clinical data and fresh fecal specimens were collected from all subjects, and the subjects’ gut microbiome was assessed using 16S rRNA gene sequencing. Multiple machine learning screens for potential biomarkers.
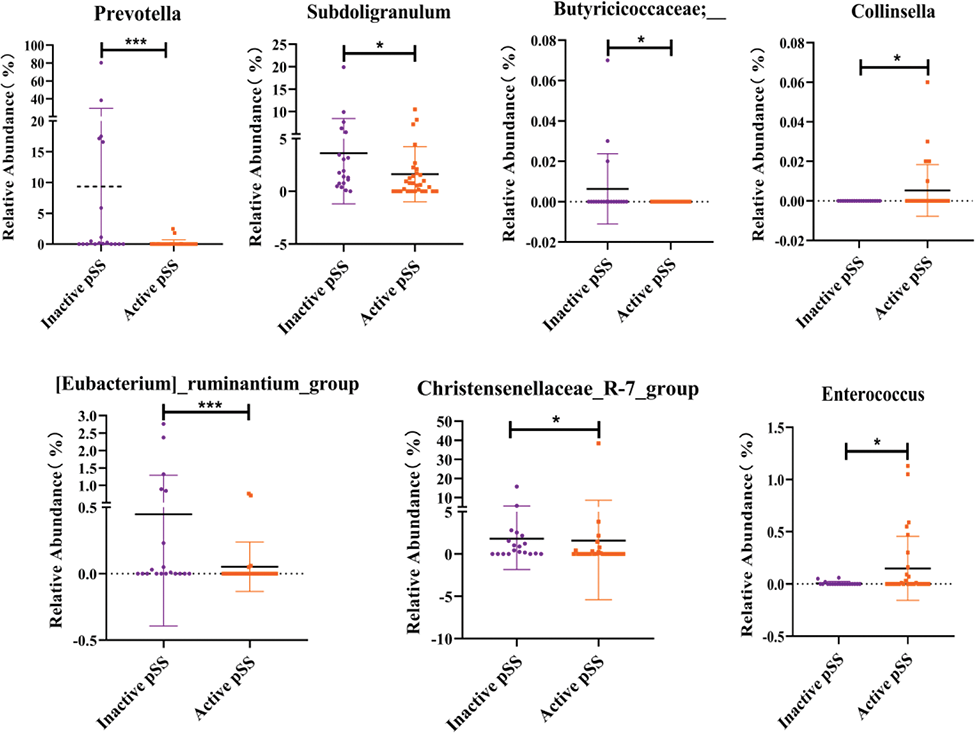
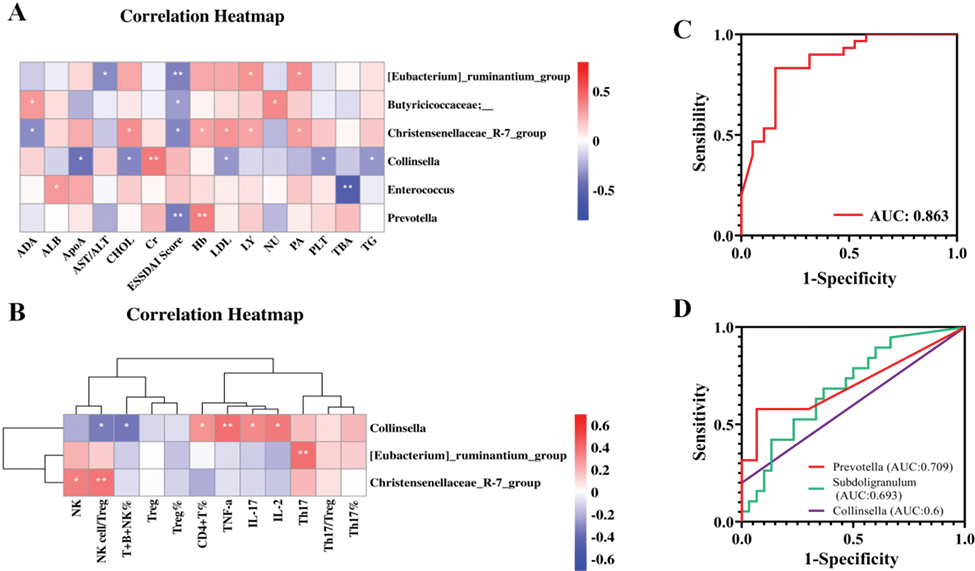
Results: We grouped pSS patients according to the ESSDAI Score and found that patients with pSS in the active group (n=30) had more severe immune imbalances and gut microbiome dysbiosis than patients with pSS in the inactive group (n=19). Moreover, there was a decrease in butyric acid-producing bacteria along with an increase in pro-inflammatory mediator-producing flora in the active pSS patients. Results of correlation analyses showed that butyric acid-producing bacteria (e.g., Prevotella, [Eubacterium]_ruminantium_group, Christensenellaceae_R-7_group, and Butyricoccaceae;_) were negatively correlated with the ESSDAI Score. In particular, Collinsella was positively correlated with the levels of cytokines (e.g., IL-17, IL-2, TNF-a) in peripheral blood, and [Eubacterium]_ruminantium_group and Christensenellaceae_R-7_group were positively correlated with the absolute number of Th17 cells and NK cells, respectively. Next, we screened three significant genera (AUC up to 0.863) as potential biomarkers for assessing disease activity using the machine learning method of Lasso combined logistic regression, which were Prevotella (AUC=0.709), Subdoligranulum (AUC=0.693), Collinsella (AUC=0.6).
Conclusion: Dysregulation of the gut microbiome is present in patients with pSS and is particularly significant in patients with active disease. A dysregulated gut microbiome may be involved in immune dysfunction in pSS patients, which in turn promotes disease progression. Therefore, a healthy gut microbiome is essential for patients with pSS, and attention to gut health may help to slow the progression of pSS disease.
Microbial communities with significant differences at the genus level in the active group compared to the inactive group.
Correlation analysis and potential biomarkers: (A) Correlation between important differential bacterial genera and conventional laboratory indicators; (B) The correlation between important differential bacterial genera and immunological indicators; (C) And (D)Diagnostic efficacy of biomarkers screened by Lasso and logistic regression.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.