

Background: Bone marrow edema (BME) and structural damage (fat metaplasia, erosions, sclerosis, backfill) on magnetic resonance imaging (MRI) of the sacroiliac joint (SIJ), qualitatively identified as sacroiliitis, are a hallmark of axial spondyloarthritis (axSpA). SIJ lesions on MRIs of postpartum women (PPW), potentially influenced by pregnancy-related mechanical stress, may complicate the distinction to axSpA. Additionally, patients with inflammatory bowel diseases (IBD) are at an increased risk of axSpA, and the impact of MRI lesions on back pain symptoms is unclear. The extent and frequency of such lesions have been inadequately described, and few existing prospective studies with small sample sizes lack clarity.
Objectives: To determine the prevalence of ‘axSpA-like’ SIJ MRI lesions in PPW and IBD cases and assess the potential role of MRI in the early detection of axSpA in these populations.
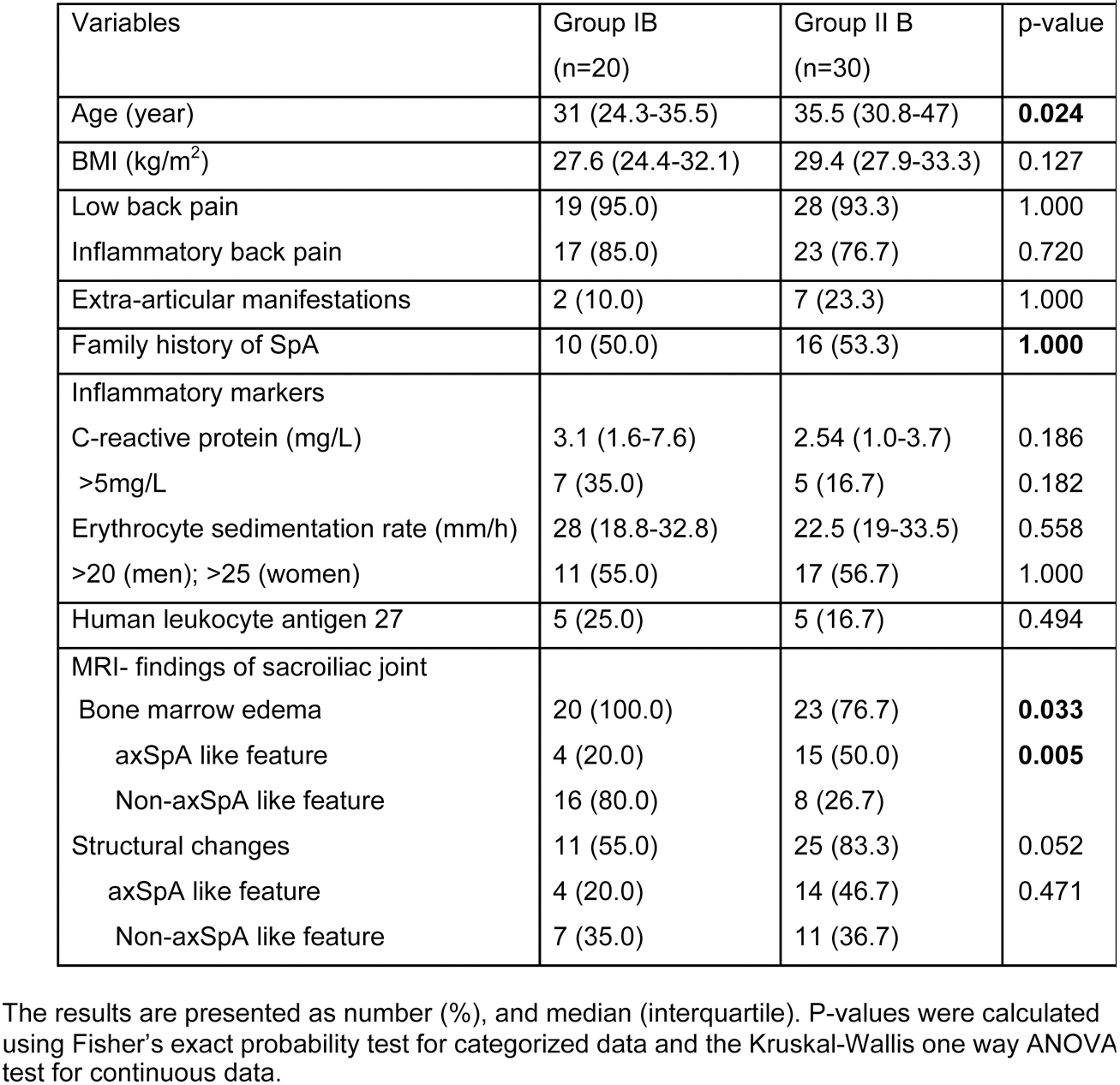
Methods: A cross-sectional study was conducted involving 173 participants (86 PPW and 87 IBD). Participants underwent comprehensive clinical, laboratory, and standardized MRI screenings of the SIJs. MR images were evaluated by three assessors. SIJ-MRI lesions were identified qualitatively using the Assessment of Spondyloarthritis International Society (ASAS) descriptions [1]. Based on MRI findings, participants were categorized into four groups: Group IA (PPW with normal SIJs), Group IB (PPW with SIJ lesions), Group IIA (IBD patients with normal SIJs), and Group IIB (IBD patients with SIJ lesions). Descriptive statistics were performed on all available parameters (significance at p<0.05).
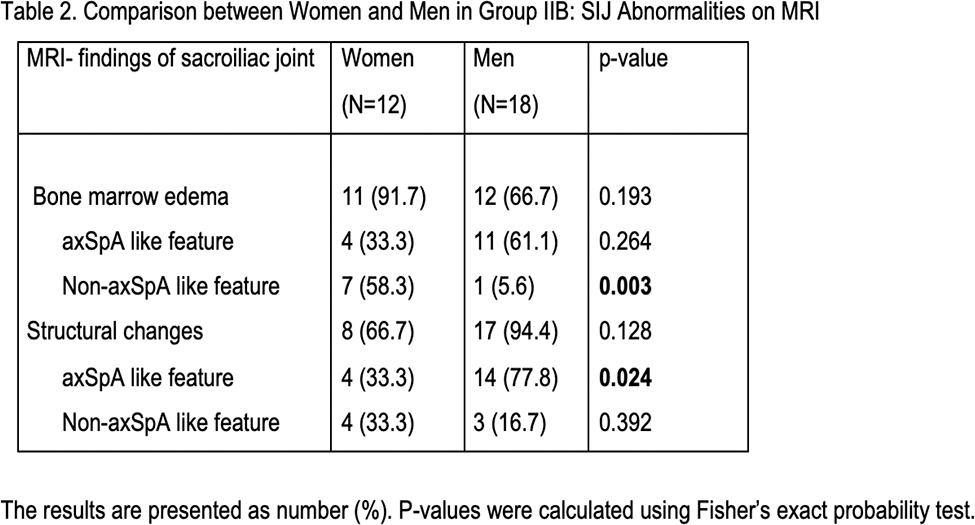
Results: SIJ-BME was prevalent in both PPW and IBD, in 23.3% and 26.4% of participants, respectively. Although both groups displayed BME, the pattern differed. In Group IB, BME was present in 100% of participants, as compared to 76.7% in Group IIB (p=0.033). While only 20% of BME in Group IB displayed axSpA features, this proportion rose to 50% in Group IIB (p=0.005). Interestingly, contrasting patterns emerged regarding structural SIJ changes. Group IIB presented a significantly higher prevalence of structural changes in SIJ compared to Group IB (83.3% vs 55%, p=0.052). The analysis of “axSpA-like” features within structural changes did not differ significantly between PPW and IBD, despite higher proportion “axSpA-like” features in IBD (46.7%) compared to PPW (20%). However, this difference did not reach statistical significance according to Fisher’s exact test (p=0.471). Although not statistically significant, women in Group IIB appeared to have a higher prevalence of BME compared to men (91.7% vs 66.7%, p=0.193). Notably, a statistically significant difference was observed in the proportion of non-axSpA-like BME between genders within group IIB, with women exhibiting a considerably higher proportion than men (58.3% vs 5.6%, p=0.024). These findings are summarized in Tables 1 and 2.
Conclusion: Despite comparable SIJ inflammation prevalence, distinct patterns emerged: PPW primarily exhibited BME, while IBD patients had a higher prevalence of structural SIJ changes. This pattern heterogeneity complicates accurate differentiation from axSpA solely on MRI, increasing the risk of misdiagnosis, potentially leading to unnecessary investigations and inappropriate treatment. Integrating clinical context, alongside cautious MRI interpretation, is crucial for precise diagnosis and optimized patient management in PPW and IBD populations. Further research is needed to refine MRI criteria for enhanced discrimination between axSpA and non-axSpA sacroiliitis in these populations.
REFERENCES: [1] Maksymowych W et al, Ann Rheum Dis 2019.
Acknowledgements: NIL.
Disclosure of Interests: None declared.