

Background: Cluster analysis (CA) serves as a foundational technique in the fields of data mining and machine learning, dedicated to uncovering intrinsic patterns within datasets. Recognized for its efficacy in partitioning data into cohesive groups, K-means finds versatile applications across various domains. Its potential impact extends to providing vital insights into clinical phenotypes, helping discern whether specific groups demonstrate higher prevalence among patients with Spondyloarthritis (SpA).
Objectives: The aim of this study was to identify and describe the different clinical phenotypes among patients with a diagnosis of axial (axSpA) and peripheral (pSpA) Spondyloarthritis from an Argentine cohort.
Methods: Multicenter cross-sectional, descriptive and analytical study. Patients ≥ 18 years old with diagnosis of axSpA or pSpA (ASAS Criteria) from 15 centers were included. Sociodemographic data, comorbidities, habits, body mass index (BMI), characteristics of SpA and treatment were recorded. Statistical analysis: descriptive statistics was estimated. CA of variable subsets determined the optimal number of patterns, with the ‘NbClust’ package employing the iterative partitioning method, K-means. Statistical tests such as Chi2, Fisher, t-Student, or Wilcoxon were applied to compare groups. P≤0.05 was considered. R 4.3.1 software was used for data analysis.
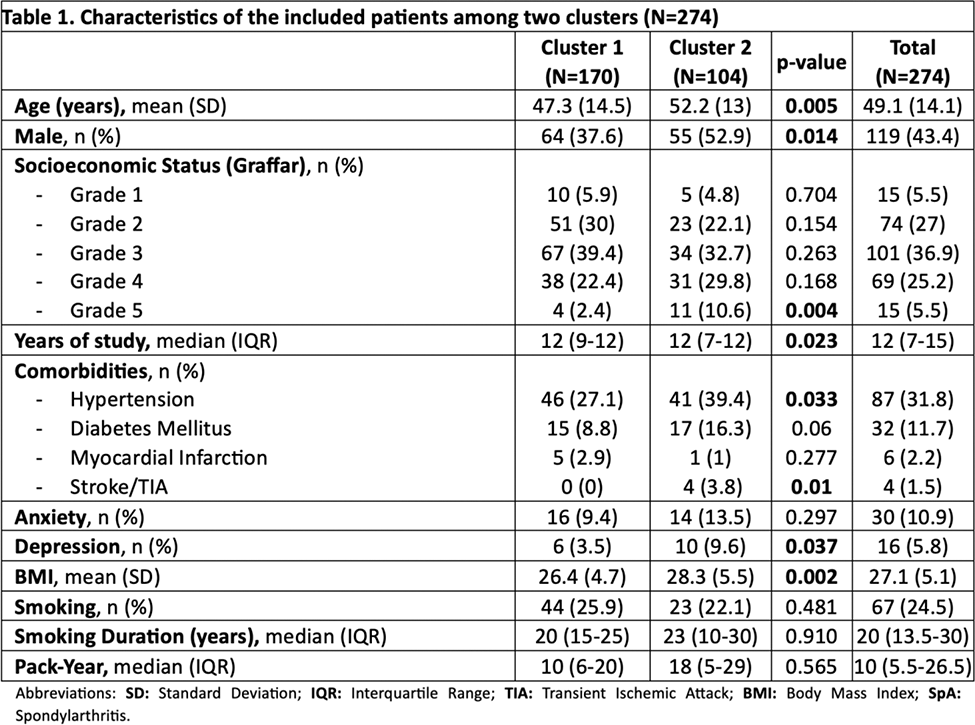
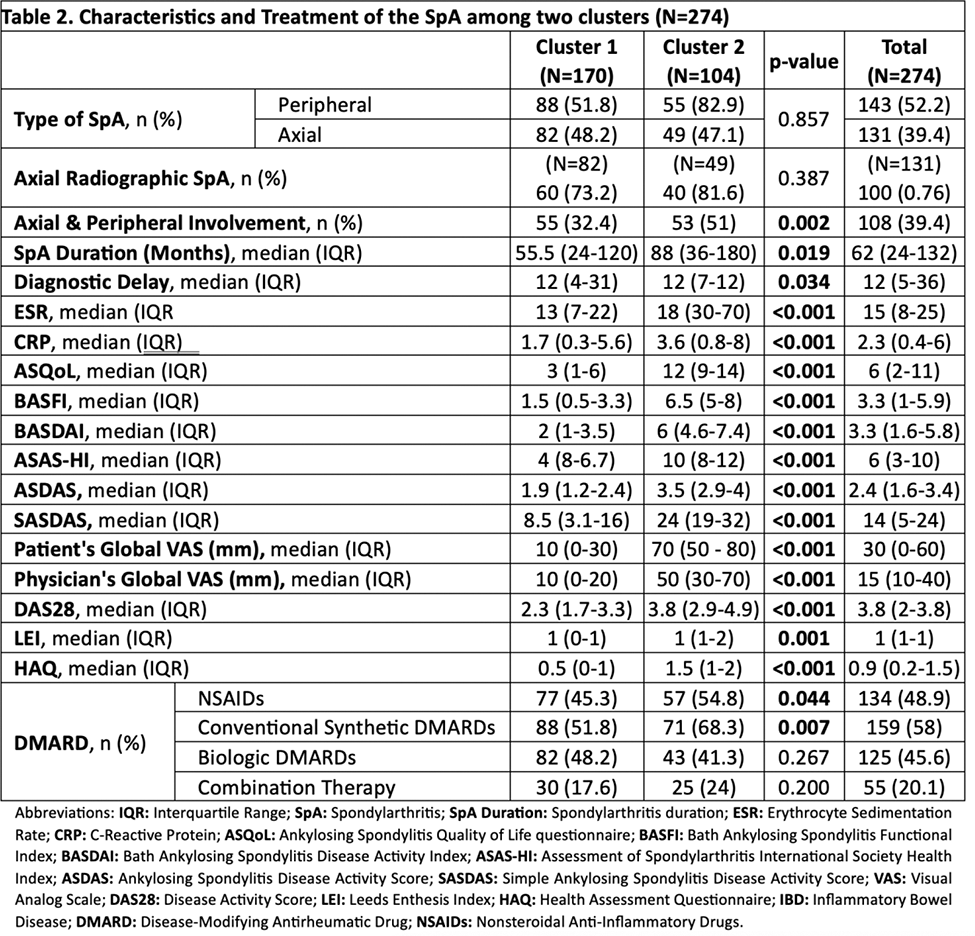
Results: The study enrolled 274 SpA patients: 43% male, mean age of 49 (±14) years, and a disease duration of 62 months (IQR 24-132). Two patient clusters emerged (Cluster1: N=170; Cluster2: N=104). Details are presented in Table 1 : Cluster 2 patients were characterized by a higher male prevalence (53% vs. 38%, p=0.014), older age (52 vs. 47, p=0.005), and lower socioeconomic status (11% vs. 2%, p=0.009). Additionally, Cluster 2 exhibited a higher incidence of hypertension (39% vs. 27%, p=0.033), depression (10% vs. 3%, p=0.037), stroke/TIA (0% vs. 3.8%, p=0.01), and elevated body mass index (BMI) (28 vs. 26, p=0.002). Details concerning SpA characteristics are shown in Table 2 : Cluster 2 displayed prolonged disease duration (88 vs. 55 months, p=0.019), greater peripheral involvement (83% vs. 52%, p=0.857), and increased axial and peripheral involvement (51% vs. 32%, p=0.002), accompanied by elevated ESR (p<0.001) and CRP (p<0.001). In terms of clinical measures, Cluster 2 demonstrated elevated scores in ASQoL, BASFI, BASDAI, ASAS-HI, ASDAS, SASDAS, physician and patient global assessments (PGA), DAS-28, LEI, and HAQ (all p<0.001). Furthermore, Cluster 2 exhibited a higher proportion of conventional disease-modifying drug treatments (68.3% vs. 51.8%, p=0.007).
Conclusion: This study successfully identified a more severe clinical phenotype, denoted as Cluster 2, distinguished by lower socioeconomic status, advanced age, a higher proportion of males, comorbidities, increased BMI, prolonged disease duration, peripheral involvement, greater disease activity, and the prevalent use of conventional DMARDs.
REFERENCES: NIL.
Acknowledgements: Bande J.M., Bosch Girard P., Cosatti M., Cosentino V., Duarte V., García L., Gamba M.J., Giorgis P., González P., González P., Kerzberg E., Marín J., Mariné J., Maldonado R.A., Nieto R., Oliver M., Oviedo L.M., Scarafia S., Schneeberger E.E., Sommerfieck F., Tapia J., Velozo E.J.
Disclosure of Interests: None declared.