

Background: Cardiovascular events have a high impact on morbidity and mortality in lupus disease. Eary-onset subclinical vascular lesions show faster progression in systemic lupus erythematosus (SLE) patients. Besides traditional and SLE-spesific cardiovascular risk factors, development of dysfunctional HDL plays a pivotal role in pathogenesis of accelerated atherosclerosis and correlates with indicators of atherosclerosis like plaque and intima-media thickness [1]. SLE patients with nephritis have increased plaque prevalence. However, studies on markers of dysfunctional HDL and its relation to plaque in different SLE subgroups are limited.
Objectives: We aimed to investigate the relationship between markers of dysfunctional HDL (Pon-1, Apo-A1, Anti-Apo A1) and subclinical atherosclerosis using carotid and femoral Doppler ultrasonography in a subgroup of SLE patients with nephritis.
Methods: 68 patients with SLE nephritis (class 4 and 5), 45 non-nephritis SLE patients and 36 healthy volunteers were included in the study. Total 139 participants underwent carotid and femoral Doppler ultrasonography and echocardiography. Serum levels of Pon-1, Apo-A1, Anti-ApoA1 were tested using ELISA.
Results: The average age was 43,08±9.6 in renal SLE patients, 41,5±11.05 in nonrenal SLE patients and 38,7±10.7 in healthy controls. Both renal SLE and non-renal SLE patients had similar median disease duration (167,4±85,3 vs 141,06±98,9 months). The female proportion across patient groups and healthy control had no difference. SLE patients with renal and non-renal involvement had both decreased Pon-1 and Apo-A1 and increased Anti-ApoA1 levels compared to healthy controls (p<0.05 for all). Biomarkers showed no statistical significance between renal and nonrenal SLE. Patients with nephritis and without had both increased intima-media thickness (IMT) compared to healthy controls and IMT correlated positively with total SLICC score. Biomarker levels showed no diagnostic value for differentiation of active and inactive disease assessed by SLEDAI. Both SLE groups had statistically significantly more either carotid and/or femoral plaque than healthy controls. Plaque prevalence showed no statistical difference among renal and nonrenal SLE patients. Renal SLE patients had higher both carotid and femoral plaque than non-renal SLE patients (p=0,02). Comparing renal and non-renal SLE patients with plaque, Pon-1 activity and Apo-A1 levels were lower and Anti-ApoA1 titer was higher in renal SLE patients without statistical significance. Biomarkers demonstrated no diagnostic value in the presence of plaque. Age and disease duration were significant variables predicting plaque presence in renal and nonrenal SLE patients (p<0.001, p<0.05).
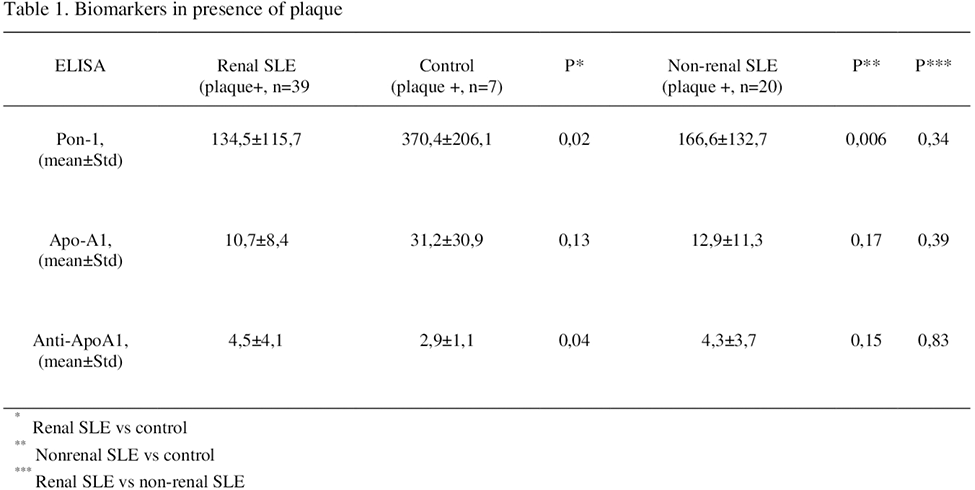
Conclusion: SLE patients with renal and non-renal involvement have both significantly increased plaque prevalence and higher intima-media thickness. Older age, longer disease duration and cumulative damage are important risk factors for plaque formation. Although a higher proportion of plaque presence was detected in patients with nephritis than in those without, the difference did not reach statistical significance. The increase in the number of patients can lead to different results. Significantly lower Pon-1 and Apo-A1 levels and elevated Anti-ApoA1 titers were demonstrated in SLE patients; however, data about their association with the presence of plaque revealed no statistical significance. Considering the contribution of proinflammatory HDL to the pathogenesis of early-onset atherosclerosis, markers of dysfunctional HDL can provide important data when used simultaneously with imaging modalities in longitudinal follow-up.
REFERENCES: [1] McMahon, Maureen et al. Arthritis and rheumatism vol. 60,8 (2009): 2428-37
Acknowledgements: NIL.
Disclosure of Interests: None declared.