

Background: The traditional inflammatory markers i.e. erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) perform poorly as markers of disease activity in Takayasu arteritis (TAK) [1]. We evaluated serum p-glycoprotein (Pgp) and a new isoform of CRP (monomeric CRP) as markers of disease activity in TAK.
To compare serum p-glycoprotein levels between TAK and healthy controls.
To compare serum p-glycoprotein levels between active and inactive TAK
To compare serum p-glycoprotein levels, traditional highly sensitive C-reactive protein (CRP) and monomeric CRP as markers of active TAK.
To compare serum p-glycoprotein levels before and after immunosuppressive treatment in a subset of treatment-naive TAK.
Methods: Adult (≥18 years) TAK patients satisfying 1990 American College of Rheumatology classification criteria or the Chapel Hill Consensus Conference definition or the American College of Rheumatology/ European Alliance of Associations for Rheumatology 2022 classification criteria for Takayasu arteritis were prospectively enrolled. Serum Pgp, CRP and monomeric CRP were measured by ELISA using commercially available kits. T lymphocyte populations in peripheral blood were characterized by using flow cytometry to identify Th17 (CD4+ IL-17+), Th17.1 (CD4+ IL-17+ IFN-γ+), and Pgp-expressing T lymphocytes (CD4+ Pgp+), all normalized to T regulatory (Treg) populations (CD4+ CD25+ FoxP3+). MDR1 and MRP1 function was assessed by flow cytometry using inhibitors Verapamil (MDR1 inhibitor) and MK-571 (MRP1 inhibitor). Disease activity in patients with TAK was assessed as per physician global assessment. Serum Pgp, monomeric CRP, CRP were compared between TAK and healthy controls, active and inactive TAK, before and after treatment in a subset of treatment-naive patients. Means with standard deviation (SD) were used to represent the data (unpaired data compared using unpaired t-test, before-after data using paired t-test). Categorical data were compared using Chi-square/ Fisher exact test, p<0.05 were considered significant.
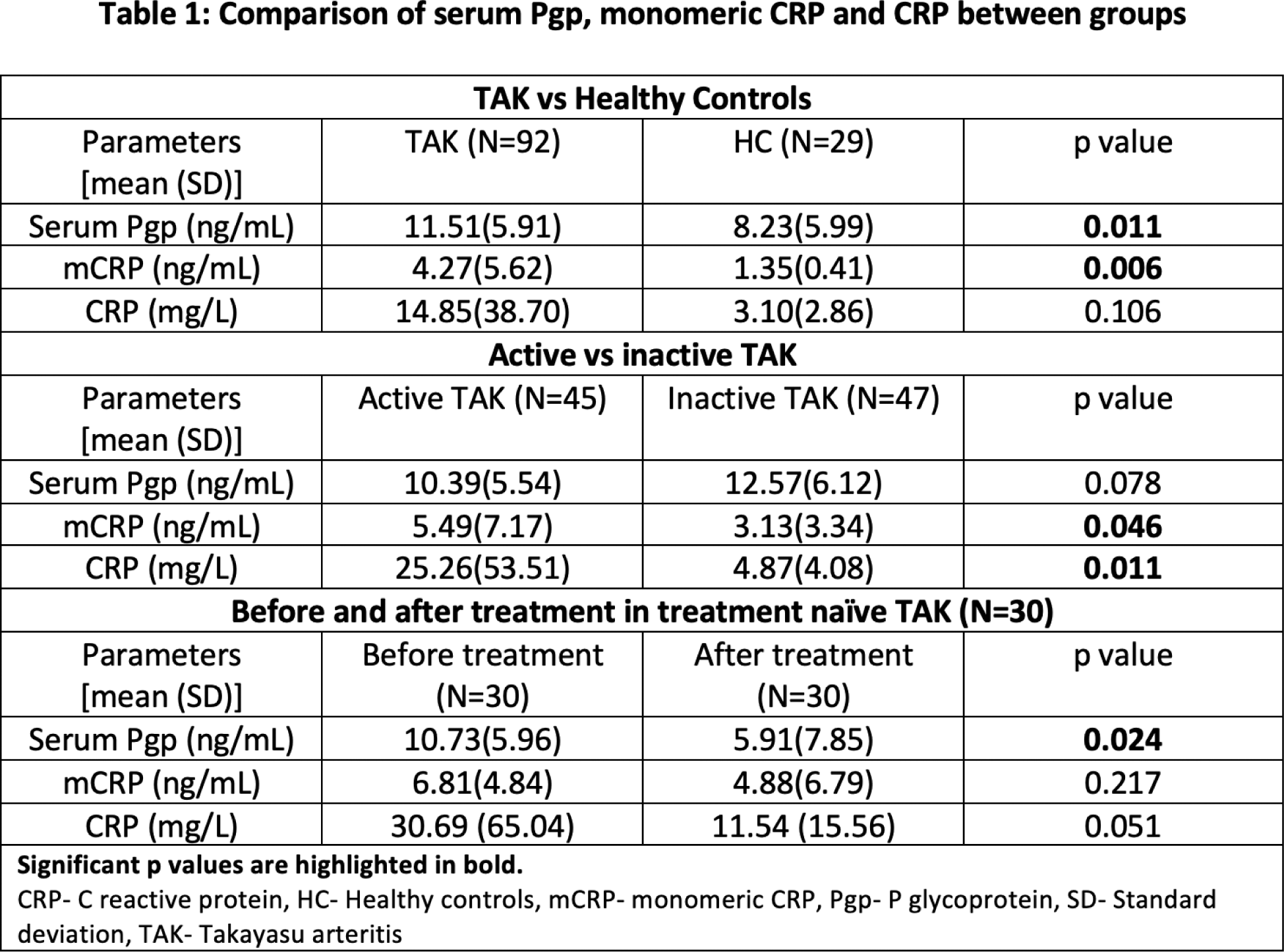
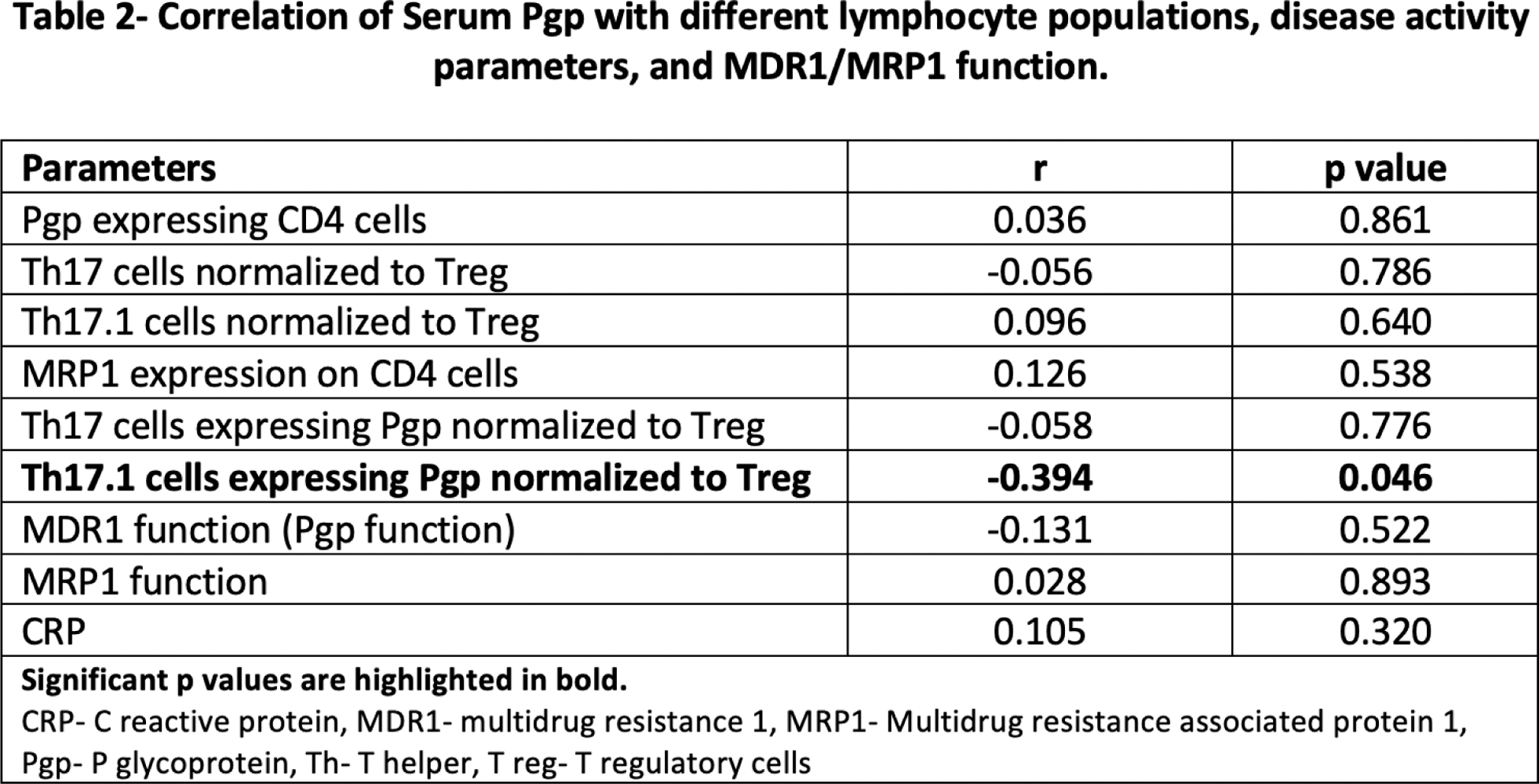
Results: Ninety-two TAK patients [63 females, mean age 33.7 (±10.9) years] were compared with 29 healthy controls [20 females, mean age 33.3 (±7.0) years]. Serum Pgp (p=0.011) and monomeric CRP (p=0.006) were increased in TAK compared to healthy controls. Monomeric CRP (p=0.046), and CRP (p=0.011) were increased in active TAK (N=45) as compared to inactive TAK (N=47). Serum Pgp levels showed a significant decrease (p=0.024) on immunosuppressive treatment for a mean period of 3.85(±2.30) months in treatment-naïve patients (N=30) (Table 1). Serum Pgp showed a weak negative correlation with Th17.1 lymphocytes expressing Pgp normalized to Treg (r=-0.394, p=0.046) but not with other cell populations (Table 2).
Conclusion: Serum Pgp and monomeric CRP are elevated in TAK patients compared to healthy individuals. Monomeric CRP is increased in active TAK. Serum Pgp levels showed a significant decrease in TAK patients on immunosuppressive therapy. The negative correlation of serum Pgp with Th17.1 lymphocytes (which are known to express Pgp) might suggest that Pgp is bound to the cell surface but not secreted in serum [2].
REFERENCES: [1] Misra DP, et al. Outcome Measures and Biomarkers for Disease Assessment in Takayasu Arteritis. Diagnostics (Basel). 2022;12(10):2565.
[2] Misra DP, Agarwal V. Th17.1 lymphocytes: emerging players in the orchestra of immune-mediated inflammatory diseases. Clin Rheumatol. 2022;41(8):2297-308.
Acknowledgements: Indian Rheumatology Association for the IRA research grant.
Disclosure of Interests: None declared.