

Background: Patients with rheumatic musculoskeletal diseases (RMDs) face an increased risk of cardiovascular (CV) diseases, cancer and infections. In Germany, general practitioners (GPs) are in charge of the general health of patients, as they are much more accessible than rheumatologists and see their patients in shorter intervals.
Objectives: To assess comorbidities, CV risk, vaccination status and cancer screening adherence of patients in an outpatient rheumatology clinic. To determine the patients’ expectations as to who is in charge of the management of their general health.
Methods: The prospective KOMO-R study recruited patients with RMDs from the outpatient Rheumatology clinic at Klinikum Nürnberg, Germany and randomized to a comorbidity information intervention or standard of care control. Here, we report results from baseline data of this study. Evaluation included EULAR suggested comorbidity screenings and vaccinations as well as national comorbidity screening guidelines for the general population [1]. All patients provided written informed consent prior to participation (ethical votum (22-113-B)).
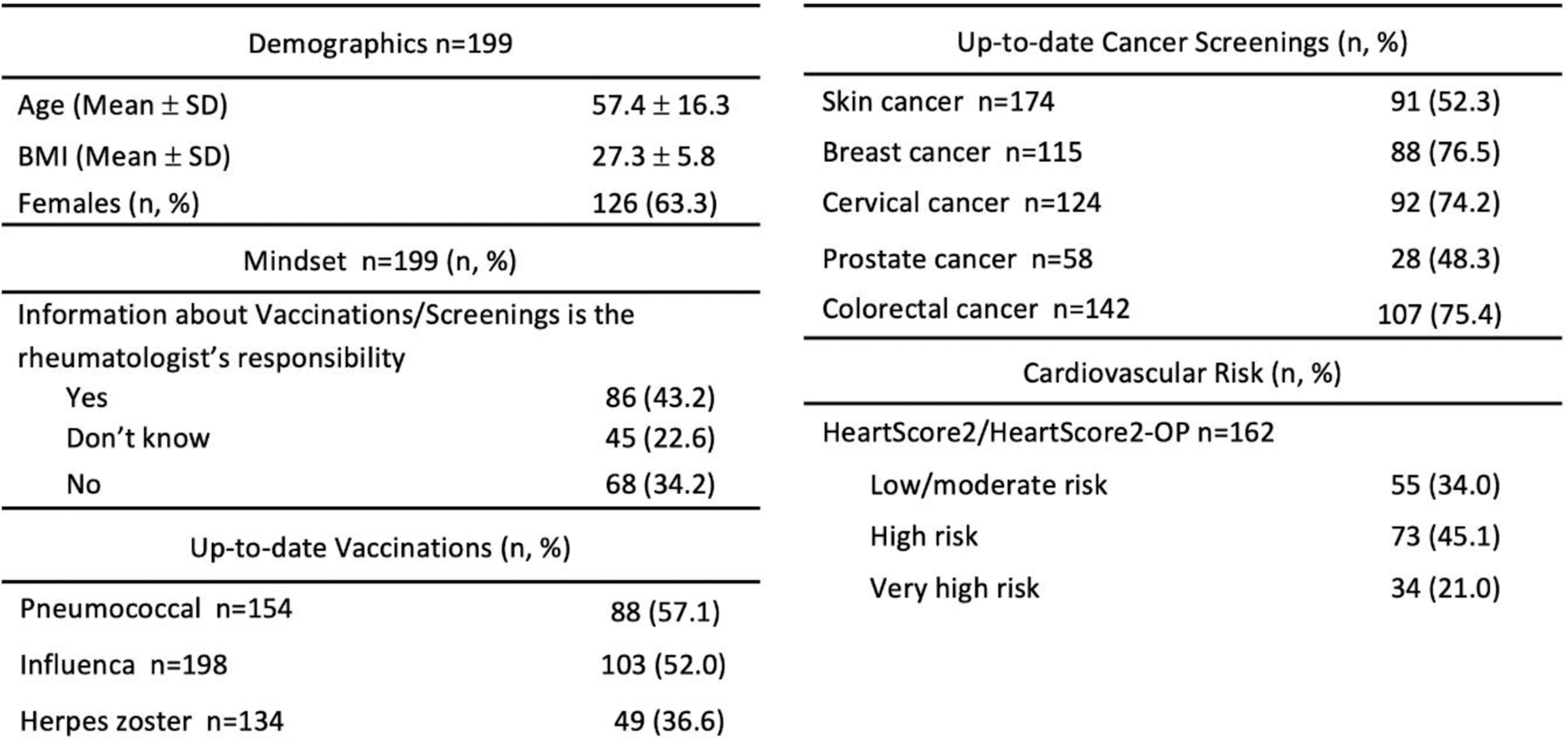
Results: 200 patients were included in the study, 199 data sets were complete at baseline. The patients were cared for by a total of 166 different GPs (baseline characteristics in Table 1). The majority (63.3%) were female and mean age was 57.4 ±16.3 (SD) years. 15.6% were active smokers. 57.1% of the study cohort had an up-to-date pneumococcal vaccination, about half of them (52.0%) had a valid flu vaccination and about one third of eligible patients (36.3%) were fully vaccinated against shingles. Gynecological and colorectal cancer screenings had the highest adherence rate (breast cancer 76.5%, colorectal cancer 75.4% and cervical cancer 74.2%) in comparison to skin cancer (52.3%) and prostate cancer screening (48.3%). A majority of patients in this study had a high (45.1%) or very high (21.0%) CV risk according to the HeartScore2/HeartScore2-OP. The majority (55.3%) was also hypertensive during at least the last two consecutive visits to the rheumatologist. 38.2% of these patients did not receive medication for their likely hypertension. As for comorbidities, about half of the 199 patients (49.7%) had a history of hypertension which they received medication for, 17.6% had a known history of high cholesterol levels which they received treatment for. About one out of ten patients had a prior CV event (11.6%) or history of serious infection requiring hospitalization (9.5%). The prevalence of depression was 16.6%. 26 out of 199 (13.1%) study participants had a history of malignancy. 43.2% of the patients stated that they believe it’s the rheumatologist’s responsibility to inform them about cancer screenings and vaccinations.
Conclusion: Our data suggests that there is an urgent need for close collaboration with GPs to optimize management of risk factors and comorbidities. Since half of the patients in this cohort were convinced that it’s the rheumatologist’s responsibility to inform them about cancer screenings and vaccinations, Rheumatologists need to manage expectations accordingly.
REFERENCES: [1] Baillet A et al. Points to consider for reporting, screening for and preventing selected comorbidities in chronic inflammatory rheumatic diseases in daily practice: a EULAR initiative. Ann Rheum Dis. 2016 Jun;75(6):965-73.
Table 1.
Acknowledgements: This study was supported by a conditional grant from Galapagos.
Disclosure of Interests: Axel Hueber Abbvie, Amgen, Galapagos, Janssen, Lilly, Novartis, Pfizer, Rheumaupdate GmbH, UCB, Abbvie, Alexion, Amgen, Janssen, Lilly, Novartis, UCB, Galapagos, Vanessa Bartsch: None declared, Kathrin Standfest: None declared, Johannes Knitza: None declared, Georg Schett: None declared.