

Background: Patients with inflammatory joint diseases (IJD), rheumatoid arthritis (RA), spondyloarthropathy (SpA), and psoriatic arthritis (PsA) are at high risk of atherosclerotic cardiovascular disease (ASCVD), and the increased risk is still present regardless of the optimized anti-rheumatic medications. Cardiovascular disease (CVD) has been reported as one of the leading causes of death among patients with IJDs as well as the general population. There is a large gap between the European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) guideline recommendations and low-density lipoprotein cholesterol (LDL-C) goal achievement in routine clinical practice.
Objectives: This study aimed to evaluate the proportion of patients with IJD with an indication for cardiovascular prevention, and the attainment of the 2019 ESC/EAS guideline-recommended LDL-C in these patients.
Methods: Patients with IJD were referred to the Preventive Cardio-Rheuma clinic for an ASCVD risk evaluation between 2019 and 2023 were included. Primary and secondary prevention with lipid-lowering treatment were initiated in patients classified as high and very high risk. The LDL-C goals for patients with high and very high risk were 1.8 mmol/L and 1.4 mmol/L, respectively, or ≥ 50% LDL-C reduction from baseline. Lipid-lowering treatment was Atorvastatin 20-40 mg or Rosuvastatin 5-40 mg, mostly in combination with ezetimibe 10 mg. The patients were followed up until the LDL-C goals were attained, with the first lipid level control 1-3 months after lipid-lowering treatment initiation, before referral to a general practitioner for follow-up.
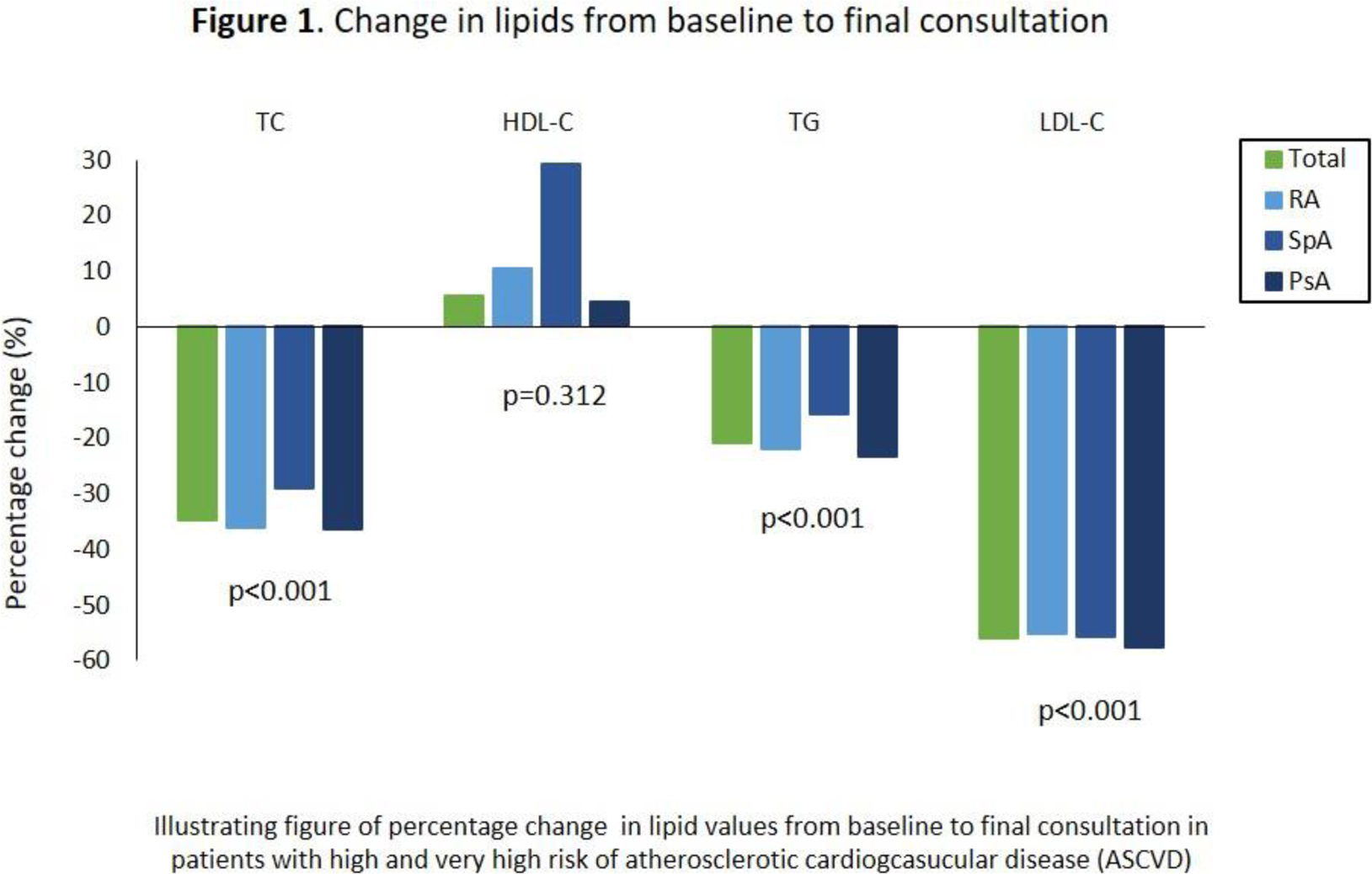
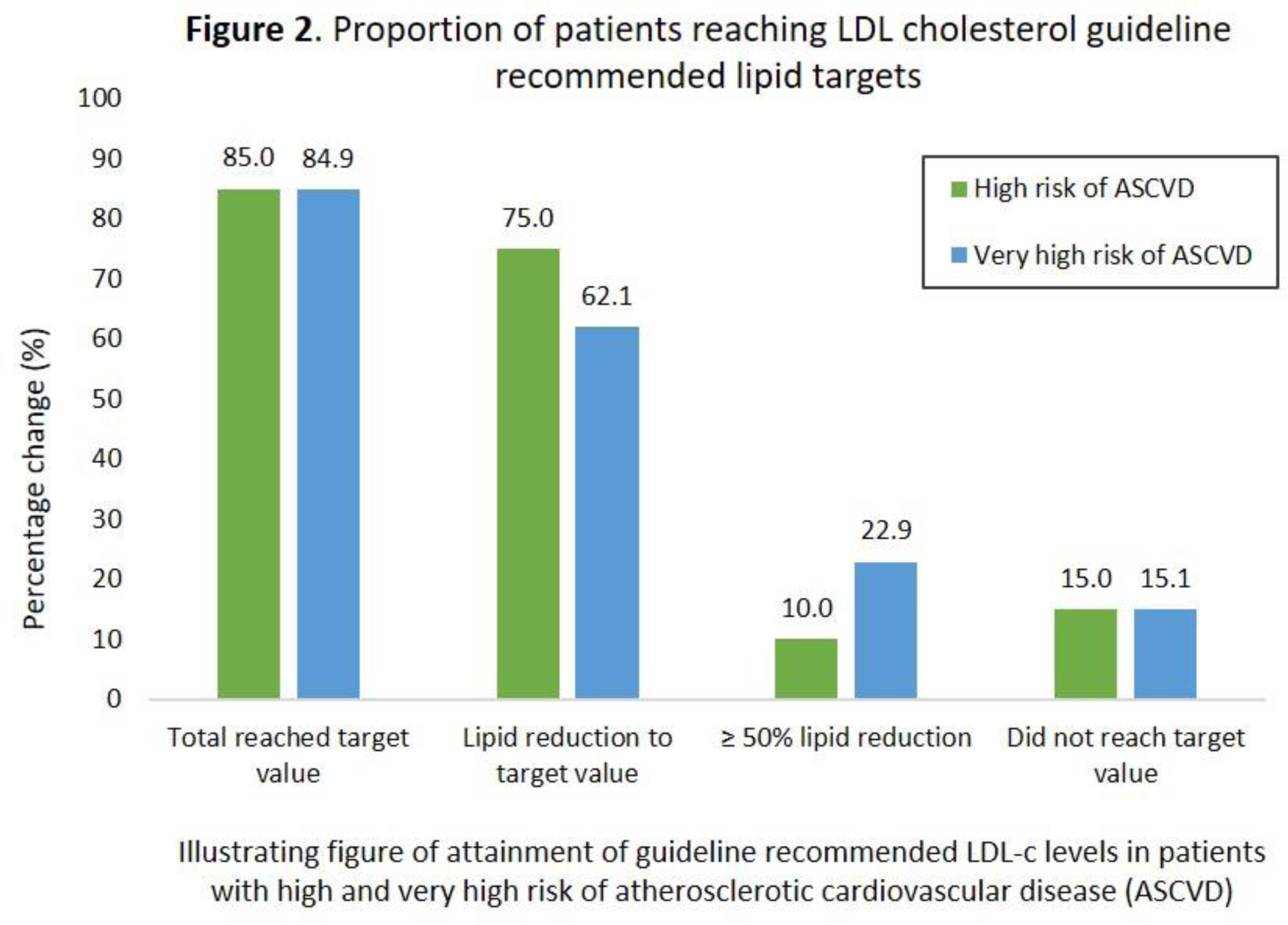
Results: In total, 186 of the 320 referred patients (RA, n=166; SpA, n=80; PsA, n=74) were classified as high (n=20) and very high (n=166) risk. The mean±SD age was 55±11.2 years and baseline LDL-C was 3.3±1.0 mmol/L in the total study population. Approximately 49% of the patients had already established ASCVD and 58% of the referred patients had an indication for initiation of lipid-lowering treatment. There was a significant reduction in LDL-C from baseline to final consultation across diagnostic groups with a mean reduction of 1.97±1.10 mmol/L, and a 56% reduction (RA 55%, PsA 56%, SpA 57%), p<0.001 (Figure 1) in patients assigned to lipid-lowering treatment. Approximately 85% attained recommended LDL-C levels, using a median (IQR) of 3 (2.0, 4.0) consultations, but of these, 16% only obtained ≥ 50% LDL-C reduction. Those who did not obtain LDL-C goals (15%) were either unwilling to take lipid-lowering medications, had co-morbidity issues or had intolerable side effects of treatment (Figure 2).
Conclusion: Recommended LDL-C goal attainment according to guidelines is achievable in a high proportion of patients with IJD on few consultations. These results indicate that frequent lipid control consultations after treatment initiation may be the key to success in LDL-C goal attainment.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: Eli J. Platou Sollerud: None declared, Eirik Ikdahl: None declared, Joe Sexton: None declared, Anne Eirheim: None declared, Anne Grete Semb AGS has received speaker fees from Merck/Schering-Plough, BMS, UCB, Pfizer/Wyeth, Novartis, Sanofi, Lilly and Women’s College Hospital, Toronto, Canada.