

Background: EORA (Elderly-Onset Rheumatoid Arthritis) defines Rheumatoid Arthritis (RA) that arises after the age of 65 years, accounting for 10-33% of all cases of RA. Psoriatic arthritis (PsA), part of the seronegative spondyloarthritis group, can also manifest in later years, even if more rarely than RA. However, Elderly Onset Psoriatic Arthritis (EOPsA) lacks a clear age definition, reported variably between 50 and 60 years old. In older age, RA and PsA exhibit less typical clinical presentations leading to potential overlaps, complicating differential diagnosis.
Objectives: Given the limited number of comparative reports, our study aims to comprehensively compare demographic, clinical and treatment characteristics of EORA and EOPsA patients undergoing methotrexate (MTX), and/or hydroxychloroquine (HCQ), and/or corticosteroid (CS).
Methods: Within our Center, a retrospective analysis was conducted on our cohort of patients undergoing MTX, and/or HCQ, and/or CS therapy, comparing a subpopulation of EORA patients with a subpopulation of EOPsA (PsA onset > 55 years old). Patients were consecutively enrolled at our dedicated outpatient clinics during a 4-month period (Sep-Dec 2023). Patients treated with bDMARDs and axial PsA patients were not included. Assessment included demographic parameters, clinical manifestations, and treatment modalities.
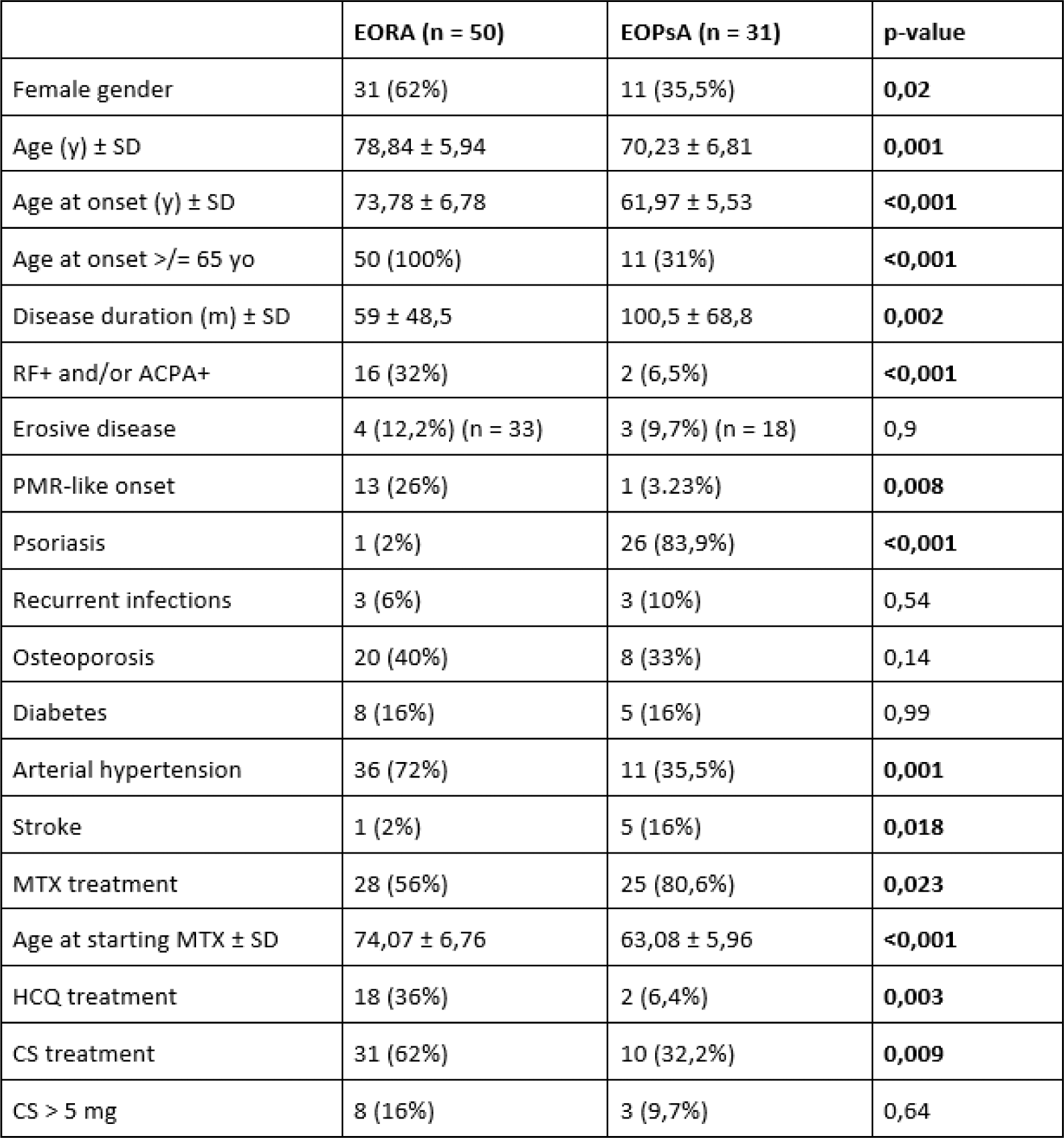
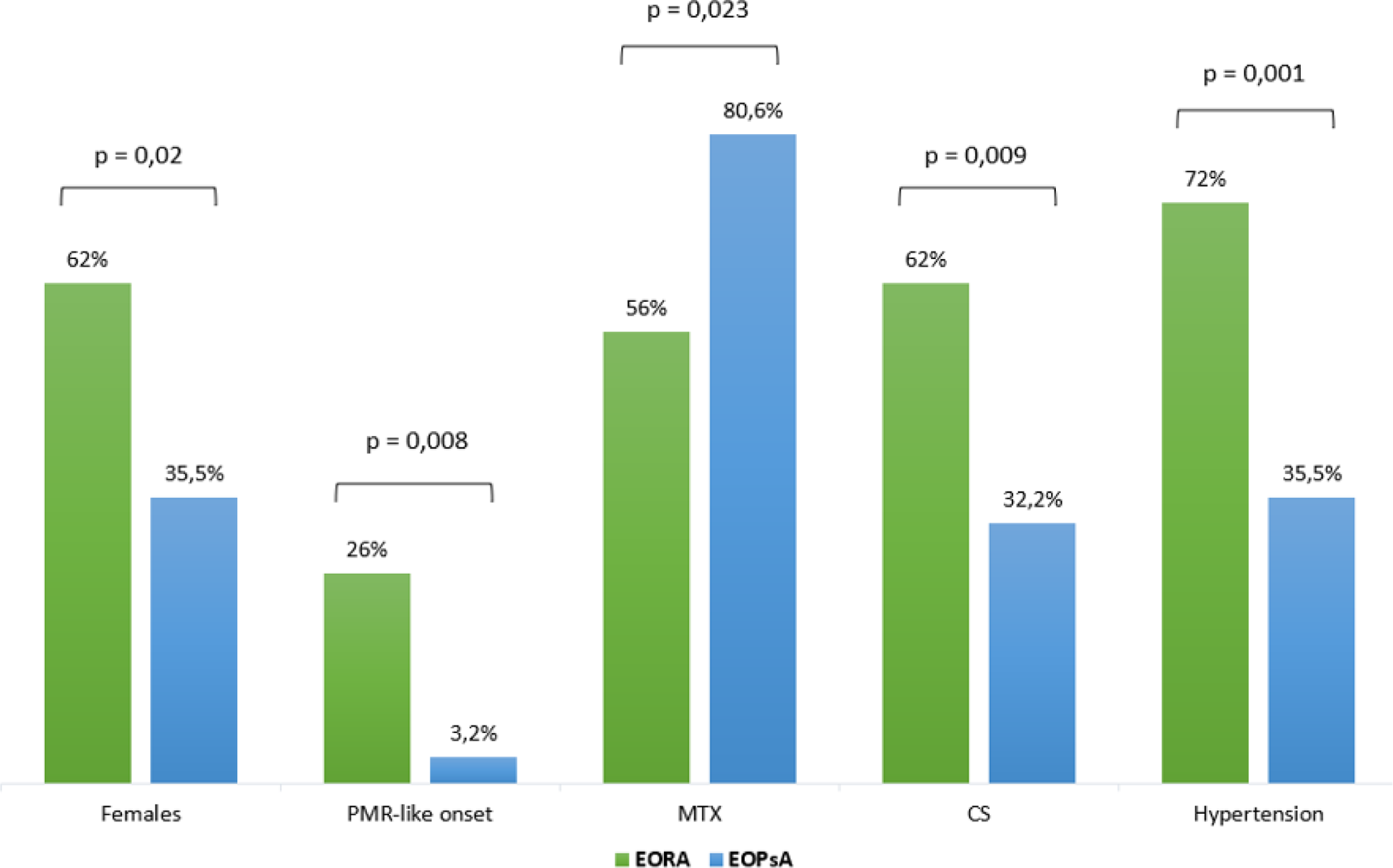
Results: During the observation period, 50 EORA patients and 31 EOPsA patients were enrolled. The demographic and clinical characteristics of the 81 enrolled patients are summarized in Table 1. Low disease activity is found in both groups, being median SDAI = 4,12 (IQR 6,07) and median DAPSA = 6,38 (IQR 8,38). Demographic characteristics reveal a gender difference, being EORA patients predominantly female (62%), while EOPsA patients predominantly male (64,5%), p = 0,02. EORA more often onsets with PMR-like symptoms (26%) compared to EOPsA (3,2%) (p = 0,008). No significant differences are noted in Charlson Comorbidity Index (CCI) or recurrent infections, but prior malignancies (p = 0,033) and stroke (p = 0,018) are more prevalent in EOPsA patients, while arterial hypertension is more common among EORA patients (p = 0,001). Notably, 56% of EORA patients but 80,6% of EOPsA patients receive MTX (p = 0,023). Conversely, EORA patients on CS, alone or with MTX, are 62%, compared to 32,2% of EOPsA patients (p = 0,009). Main differences between the two groups are shown in Graph 1. Among patients treated with MTX, the time between diagnosis and initiation of therapy does not statistically differ between groups, being 16,04 ± 15,07 months for EORA patients and 21,96 ± 19,02 months for EOPsA patients (p = 0,37). Among EORA patients, there is a statistically significant association between ACPA positivity (14 patients, 28%) and MTX therapy (p = 0,028). There is no association between treatment with MTX at any dose and increased incidence of recurrent infections (p = 0,64). Conversely, an association is found between CS therapy and recurrent infections (p = 0,011).
Conclusion: Gender disparities and different onset characteristics exist between EORA and EOPsA patients. A different therapeutic attitude emerges between the two groups, EORA patients being more frequently on CS therapy and EOPsA patients on MTX. This could be explained by the fact that cutaneous psoriasis, present in the vast majority of EOPsA patients, benefits from treatment with methotrexate; furthermore, the higher frequency of PMR-like onset among EORA patients could explain the persistence of treating these patients with CS even after long disease course. It is useful to note, however, that there are no differences in terms of recurrent infections between the two groups, while patients under CS, but not MTX, more frequently suffer from recurrent infections. Furthermore, arterial hypertension is more common among EORA patients, who are treated more often with CS. These findings suggest a potential benefit for more EORA patients to receive MTX, in order to reduce or stop CS therapy.
REFERENCES: NIL.
Table 1. Demographic and clinical characteristics of EORA and EOPsA patients.
Main differences between EORA and EOPsA patients.
Acknowledgements: NIL.
Disclosure of Interests: None declared.