

Background: Growing evidence indicate substantial psychiatric comorbidity in patients with inflammatory arthritis (IA) [1]. Mental disorders may, then, subsequently contribute to worsened therapeutic response in people with rheumatoid arthritis (RA) or axial spondyloarthritis (axSpA).
To assess the occurrence of mental disorders in IA patients treated in a tertiary centre using the Mini-International Neuropsychiatric Interview (M.I.N.I.).
To investigate help-seeking for mental disorders and attitudes towards to it in IA patients.
To assess the association between symptoms of depression and anxiety and disease activity in IA patients.
Methods: This is a cross-sectional study, consisting of IA patients (RA and axSpA) drawn from daily care in an outpatient clinic. Individuals without systemic disease were invited as controls. Disease activity was assessed using ASDAS and DAS28, while patient-reported outcomes (PRO´s) were assessed using 5D-EQ, BASDAI, BASFI, and HAQ. The Czech version of M.I.N.I. (version 5.0.0) was used to screen for depression, dysthymia, suicidal ideation, hypo/manic episodes, panic disorder, psychotic disorder, and generalised anxiety disorder. Individuals scoring positively on M.I.N.I. were offered services for their mental health needs. Beck Depression Inventory (BDI-II) and Beck Anxiety Inventory (BAI) were used to assess the presence of symptoms of depression and anxiety, respectively.
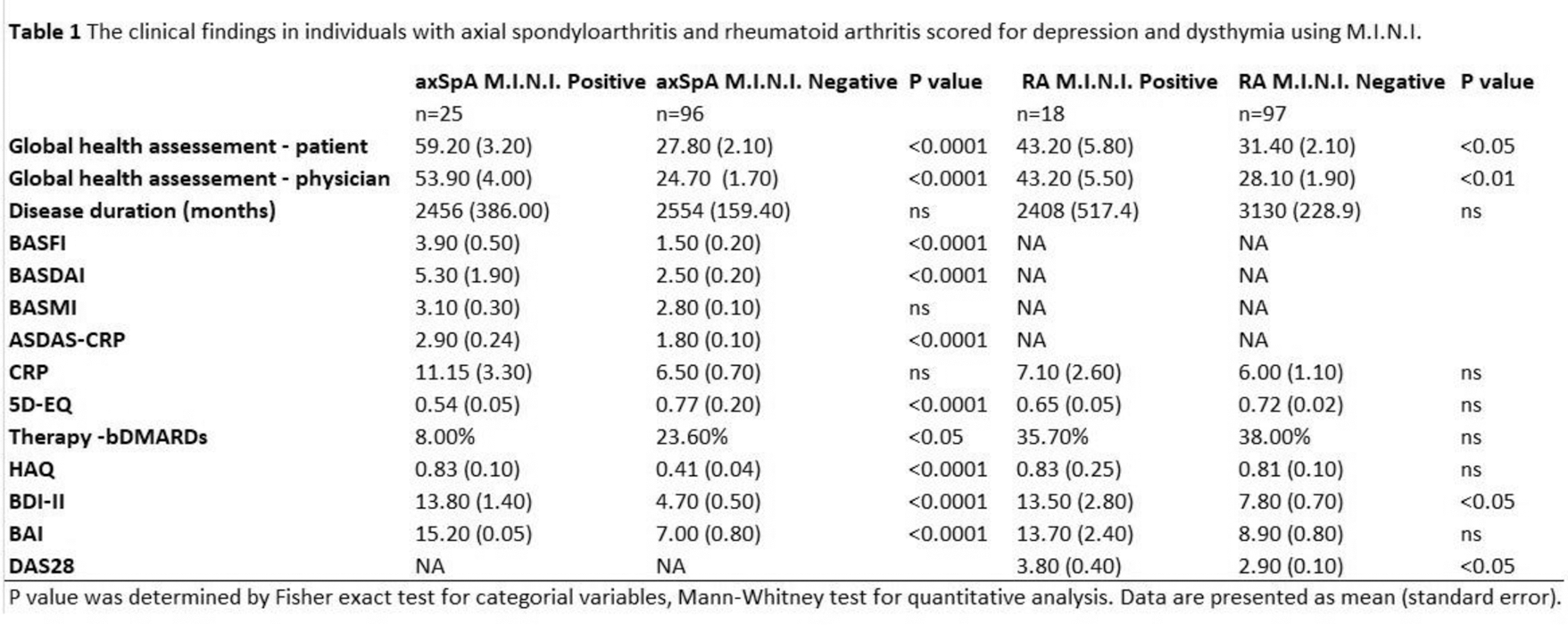
Results: The data consisted of 405 individuals: 236 with IA and 169 age- and sex-matched controls (Table 1). Approximately 30% of patients with IA scored positively on M.I.N.I. for at least one of the studied mental disorders, most commonly for depression, dysthymia, and suicidal ideation (Table 1). However, the majority of IA patients who scored positively on M.I.N.I. refused the offered services for their mental health needs (Table 1). The main reasons for not seeking help were waiting for a potential further deterioration of mental health before considering seeking help (43.10%), postpone (16.70), and belief that professional help is not needed for their mental health needs (13.90%). Both axSpA and RA patients had, on average, higher scores on BDI-II (6.12±0.60 and 7.90±0.70 vs. 3.05±0.12; all p<0.0001) and BAI (7.30±0.80 and 9.20±0.70 vs. 4.16±0.30; all p<0.0001) than the control group. ASDAS-CRP positively correlated with BDI-II and BAI in axSpA patients (r=0.507 and r=0.481; all p<0.0001). However, in RA patients, the correlation between BDI-II and BAI and DAS28 was relatively weak (r=0.264 and r=0.254, all p<0.01).
Conclusion: Despite profound psychiatric comorbidity in axSpA and RA patients and positive association between symptoms of depression and anxiety and disease activity, help-seeking for mental health is seriously lacking. Our study highlights the importance of facilitating the provision of mental health services to IA patients.
REFERENCES: [1] Howren A, et al. Arthritis Care Res (Hoboken). 2024 Jan 8. DOI: 10.1002/acr.25294.
[2] Sheehan DV, et al. J Clin Psychiatry. 1998;59 Suppl 20:22-33;quiz 34-57.
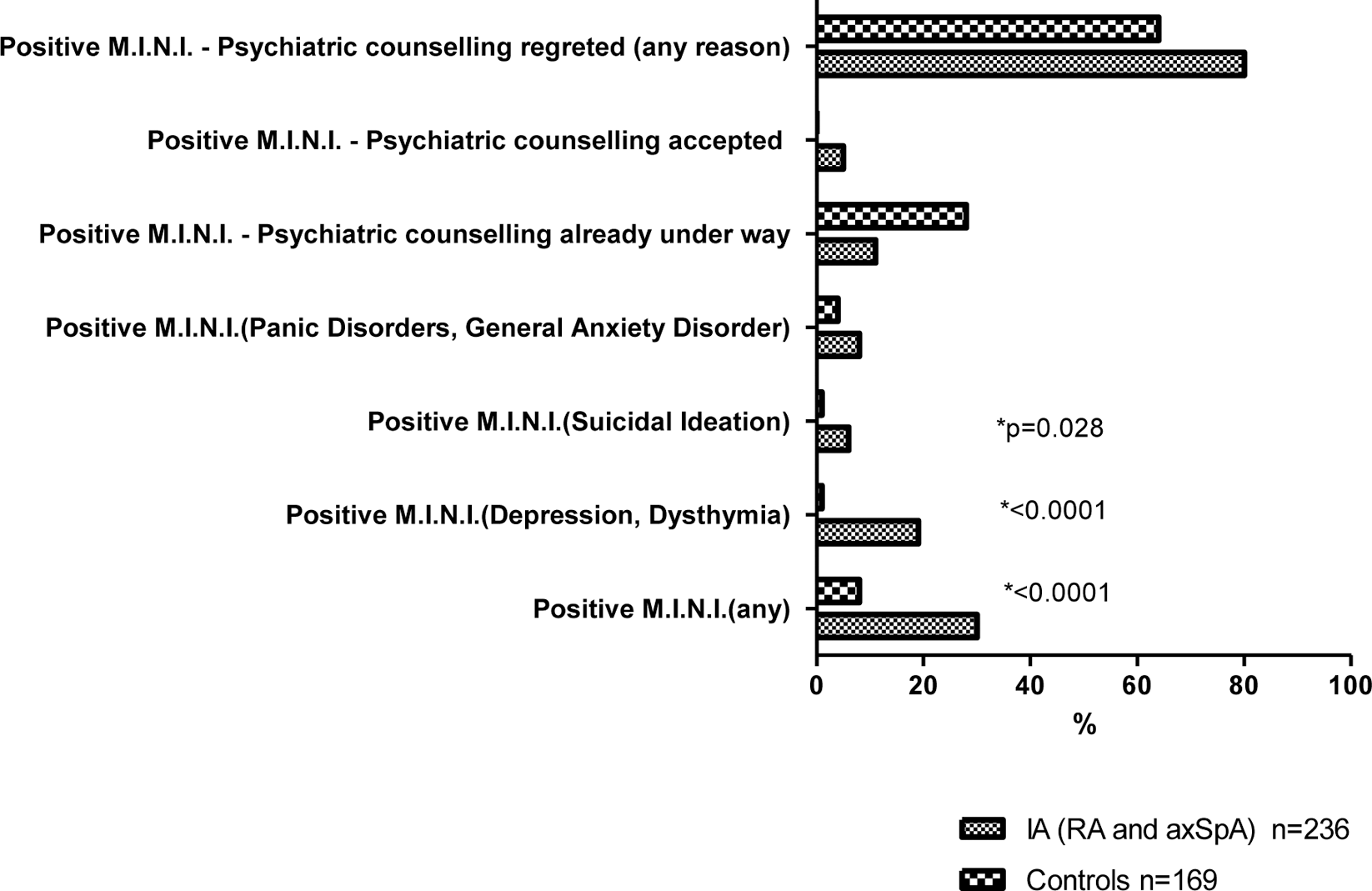
Graph 1. The M.I.N.I. outcomes in people with inflammatory arthritis and healthy individuals
Acknowledgements: Czech Health Research Council: NU21-09-00297.
Disclosure of Interests: None declared.