

Background: High Resolution Computed Tomography (HRCT) is commonly used to evaluate respiratory symptoms and assess for the possibility of interstitial lung disease (ILD) in patients with connective tissue diseases (CTDs) – rheumatoid arthritis (RA), systemic sclerosis (SSc), Sjorgrens (SJO), dermato-myositis/polymyositis (DM/PM), and systemic lupus erythematosus (SLE). It is unclear whether periodic HRCT can be routinely used to examine individual’s morbidity/mortality risk, and how evaluation can guide treatment.
Objectives: We conducted a scoping review in PubMed to enable description of HRCT characteristics of CTD-ILD and assess whether there are differences that provide insight regarding pathobiology and predict morbidity/mortality.
Methods: We searched PubMed (1993 thru end 2021) for articles reporting data on HRCT and CTD/ILD features in RA, SSc, SJO, DM/PM, and SLE, using mesh terms: HRCT ILD findings in RA/SSc/SJO/DM/PM/SLE, HRCT ILD predictors of survival/mortality in RA/SSc/SJO/DM/PM/SLE. Inclusion criteria: studies in English, data for chest HRCT, human study participants 18 years or older, not a review article, reporting results for at least one CTD, data separable for extraction if more than one disease was included. Exclusion criteria included non-English, animal or/and in vitro data only, and lack of separability into the diseases of interest. We accepted the diagnoses as given, not requiring that the diseases met ACR/EULAR classification criteria, nor explicitly describe HRCT technique. Article bias was measured using the Effective Public Health Practice Project (EPHPP) tool for standarized assessment of study quality. Data for ILD patterns of interest – usual interstitial pneumonitis (UIP) or nonspecific interstial pneumonitis (NSIP), with or without reticulation, bronchiestasis, honeycombing, or/and groundglass appearnce - were extracted into a standardized case report form and entered into an Excel spreadsheet for analysis.
Results: A total of 483 publications were identified and 110 analyzed. According to Effective Public Health Reporting Project (EPHPP) scoring, global ratings (verified by two reviewers) were:10% strong, 30% moderate, and 60% weak.
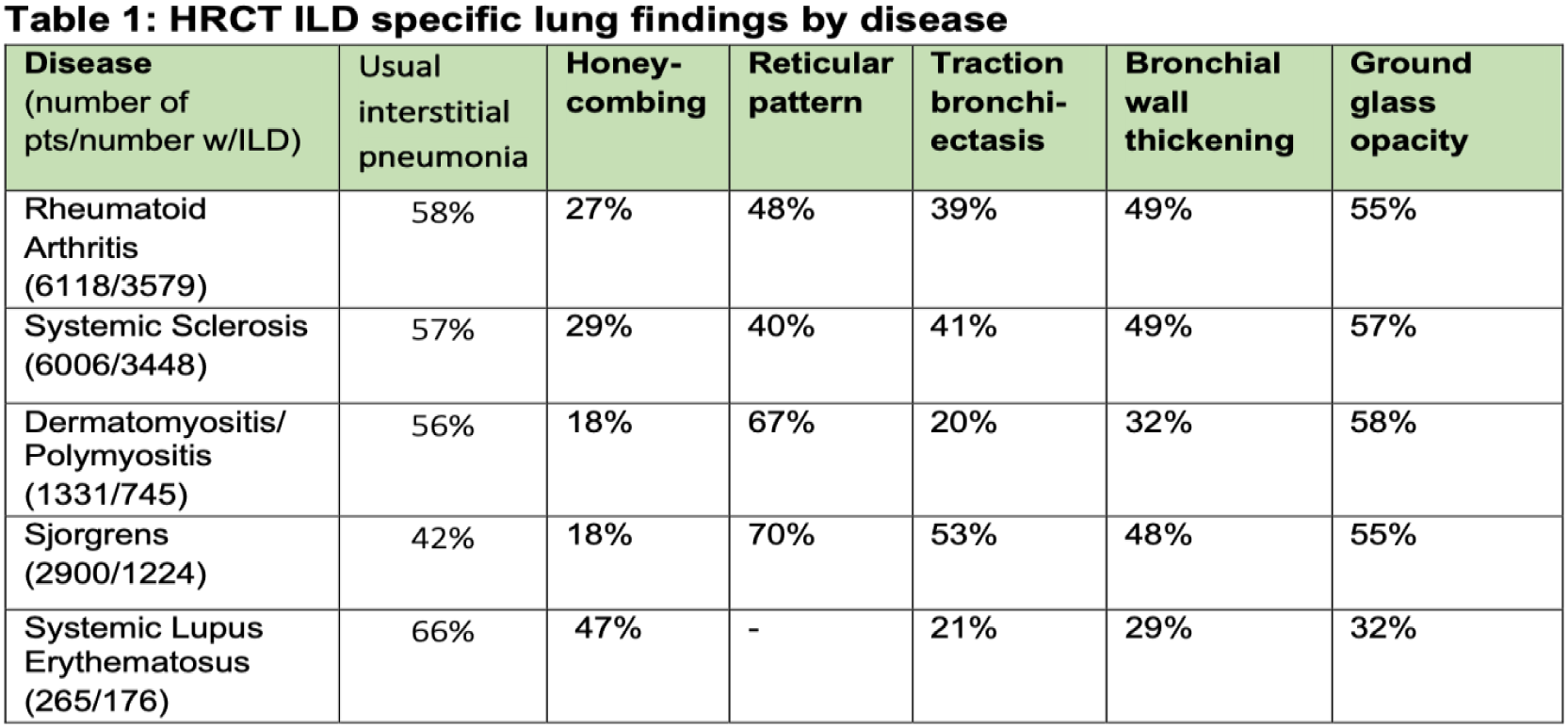
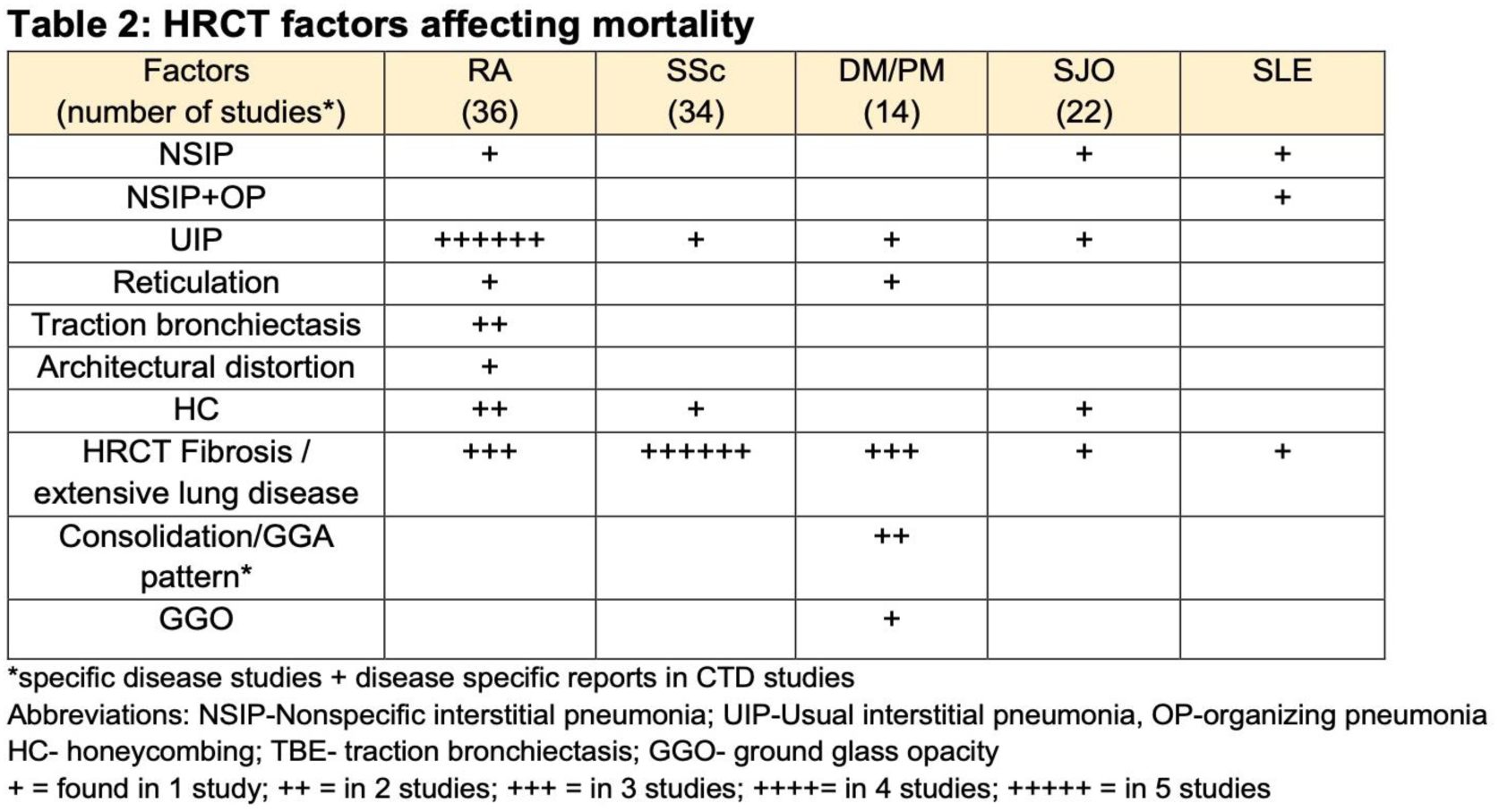
Across 21 studies reporting ILD in RA patients, prevalence was approximately 32%, evidenced by a predominant usual interstitial pneumonia (UIP) pattern, with bronchial wall thickening, a reticular pattern, traction bronchiectasis, and ground glass opacity. The presence of UIP was significantly associated with morbidity/mortality. In contrast, across 29 studies SSc patients, ILD was present in 49%. Only 6 studies analyzed ILD patterns, showing a predoiminance of non-specific interstitial pneumonia (NSIP), with traction bronchiectasis, a reticular pattern, and ground glass opacities. Higher ILD burden and baseline lung fibrosis were associated with morbidity/mortality. For DM/PM, we identified identified 12 srudies with ILD/HRCT data. ILD was diagnosed in 38% of patients, with NSIP being the predoiminant pattern with some basal consolidation, traction bronciectasis, and ground glass opacities. Similarly, in Sjorgrens, ILD was found in 37% of patients with prevalence of NSIP in 51% of those, with lymphocytic interstitial pneumonia diagnosed in 7% and UIP in 17%. Presence of these features were associated with morbidity/mortality. Finally, we found only 7 studies reporting HRCT findings for only 265 patients. Manifiestations included pleuropulmonary involvement – pleuritis, organizing pneumonia, brochiectasis, and rare alveolar hemorrhage.
Relevant overall results are shown in Tables 1 and 2.
Conclusion: HRCT can assist in diagnosis and monitoring of ILD in CTDs. Although only a small number of studies examined whether HRCT features can predict morbidity/mortality, it appears that periodic examination could be useful in this regard. More research is needed.
REFERENCES: [1] Raghu G, Remy-Jardin M, Richeldi L, et al. Idiopathic Pulmonary Fibrosis (an Update) and Progressive Pulmonary Fibrosis in Adults. Am J Respir Crit Care Med vol 205, pp e18-e47.
Acknowledgements: NIL.
Disclosure of Interests: None declared.