

Background: Interstitial Lung Disease (ILD) is characterized by progressive scarring of lung tissue, often leading to inflammation and extensive fibrosis. Various systemic autoimmune diseases, including systemic sclerosis (SSc), rheumatoid arthritis (RA), and idiopathic inflammatory myopathies (IIM), are closely linked with ILD, presenting substantial challenges in treatment and management. Despite current therapeutic interventions offering limited success, there is an urgent need for innovative and more effective strategies.
Objectives: We conducted a systematic literature review to investigate the potential of Janus kinase inhibitors (JAKi) in the context of ILD associated with systemic autoimmune diseases (SADs). The review aims to elucidate the efficacy and safety profile of JAK inhibitors, providing valuable insights into their role as a promising therapeutic approach for mitigating lung inflammation and preventing the progression of fibrosis.
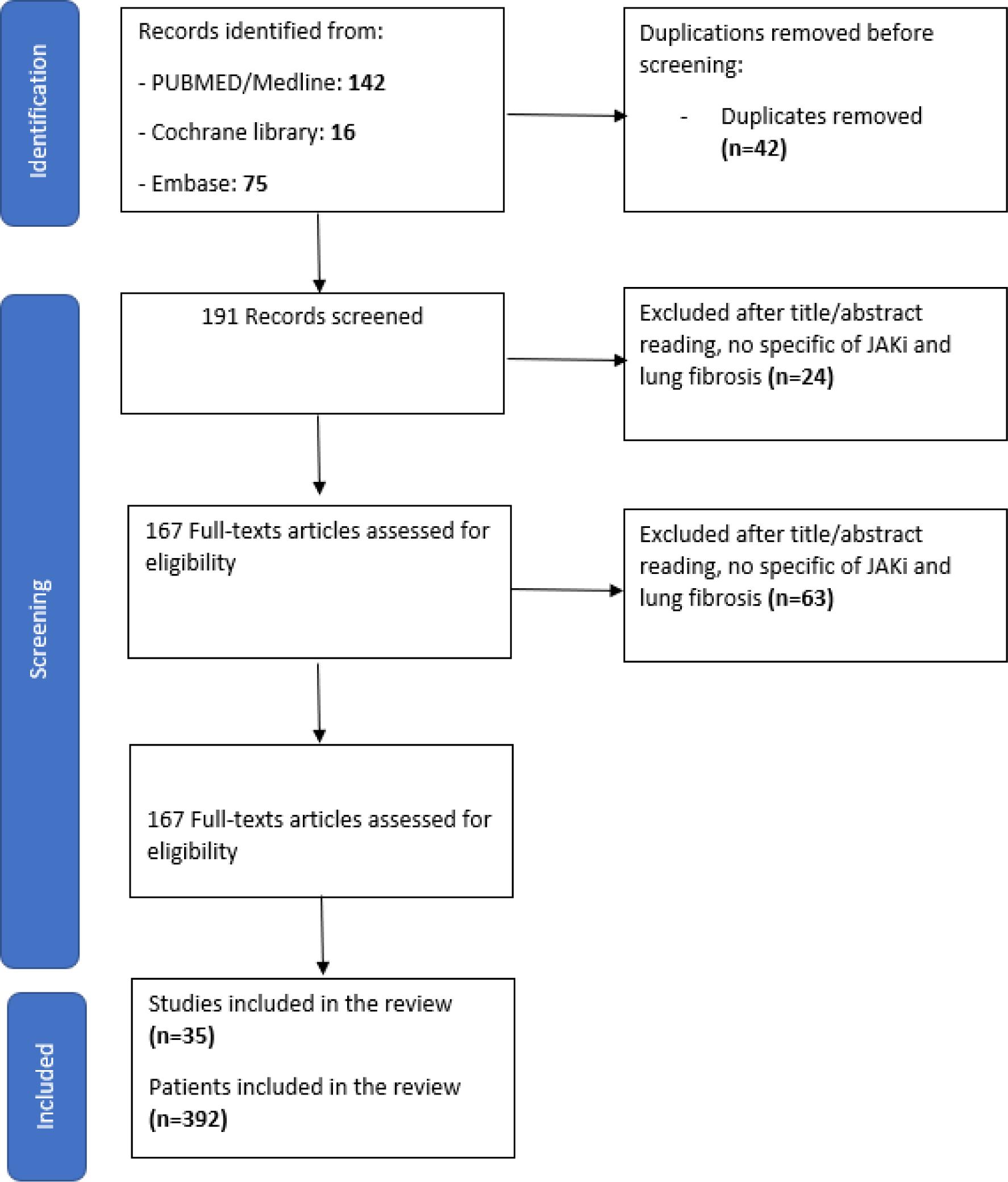
Methods: The systematic literature review followed PRISMA guidelines and was carried out using Medline, Cochrane Library, and Embase scientific databases SADs-ILD patients treated with JAK inhibitors were included-
Results: A primary search identified 233 references, with 167 studies selected for full-text review (Figure 1). Among the selected articles were 15 case reports, 5 cohort studies, 4 case controls, 1 randomized clinical trial, 10 systematic reviews, and 9 case series. In total, 392 patients (mean age 54.6±20 years) with a median treatment duration of 8 (1-54) months were included. Tofacitinib was prescribed in 279 (71%) patients, Baricitinib in 104 (27%) patients, and Upadacitinib in 3 (0.8%) patients. 221 (56%) patients had rheumatoid arthritis, 140 (36%) had inflammatory myopathies, 29 (7%) had systemic sclerosis in 29 (7%), and 2 (0.5%) had Sjögren’s syndrome. JAK inhibitors were prescribed as first-line therapy in 4 studies, involving 122 patients (31%). Combination with conventional synthetic DMARDs (csDMARDs) was used in 124 (31%) patients. Non-specific interstitial pneumonia (NSIP) and usual interstitial pneumonia (UIP) were the most frequent patterns (32.5%). Among patients with ILD, 20 studies (57%) showed no ILD progression during follow-up (7 studies with missing data, 71 patients). Improvement or stabilization of ILD imaging (72%) and FVC or DLCO (40%) were described, regardless of the pattern of lung involvement. Twenty-three patients (6%) experienced infections, which was the main cause for treatment withdrawal.
Conclusion: While conclusions from this analysis are limited due to differences in assessments across publications, overall treatment of patients with SADs with a JAK inhibitor was associated with a significant improvement in ILD. Our systematic literature review suggests that JAK inhibitors may be a viable treatment option for SADs patients with ILD, and randomized controlled trials are necessary to confirm these findings.
REFERENCES: NIL.
Flow chart of included studies
Acknowledgements: NIL.
Disclosure of Interests: None declared.