

Background: Telemedicine (TM) has strengthened its place in daily clinical practice. Teledermatology (TD) leads the way in TM due to the ability to perform visual diagnosis [1]. Rheumatologists encounter patients with skin lesions including inflammatory dermatoses, connective tissue diseases, vasculitis, panniculitis and also infectious skin lesions due to immunosuppressive treatments [2,3]. We observed that rheumatologists use TD consultations frequently when they examine patients with skin lesions in their daily practice.
Objectives: The main objective of the study was to assess the compatibility of TD with definitive diagnoses in patients with rheumatological diseases and also to investigate the diagnostic validity of rheumatologists for skin lesions they frequently encounter.
Methods: The study included patients with rheumatologic diseases who reported active skin lesions during follow-up. A rheumatologist first evaluated each patient, and a preliminary diagnosis of the skin lesion was recorded. Following, the images of the skin lesions were shared with two dermatologists and preliminary diagnoses were documented. The patients were then referred to a dermatologist for a face-to-face (FTF) visit and a final diagnosis was made by using additional tests or skin biopsies if needed. After six months, the same images of the lesions were evaluated by one teledermatologist again, blind to the final diagnosis. The validity and reliability of teledermatology were assessed. Also the positive predictive values were calculated for the teledermatologists and rheumatologists.
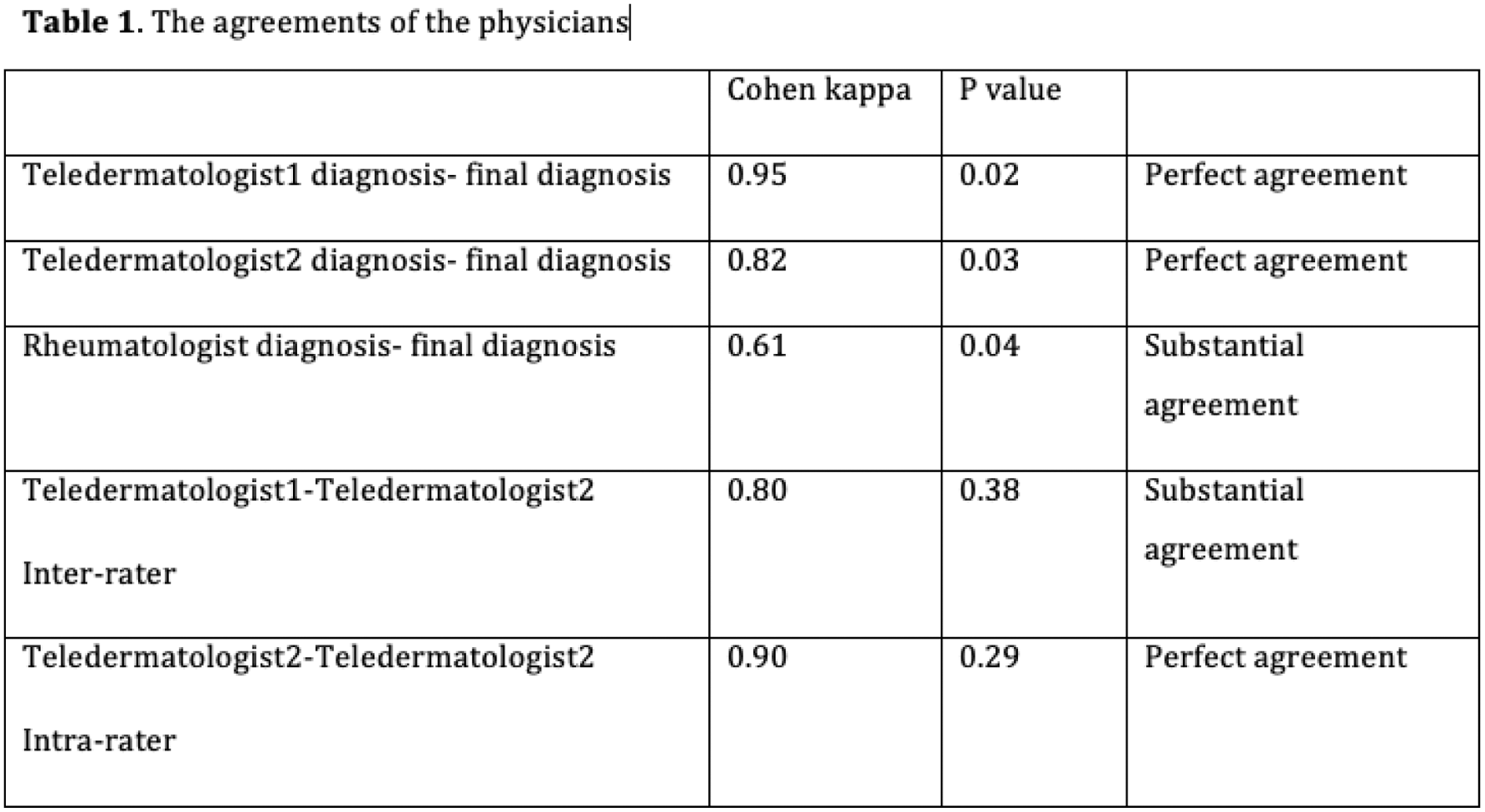
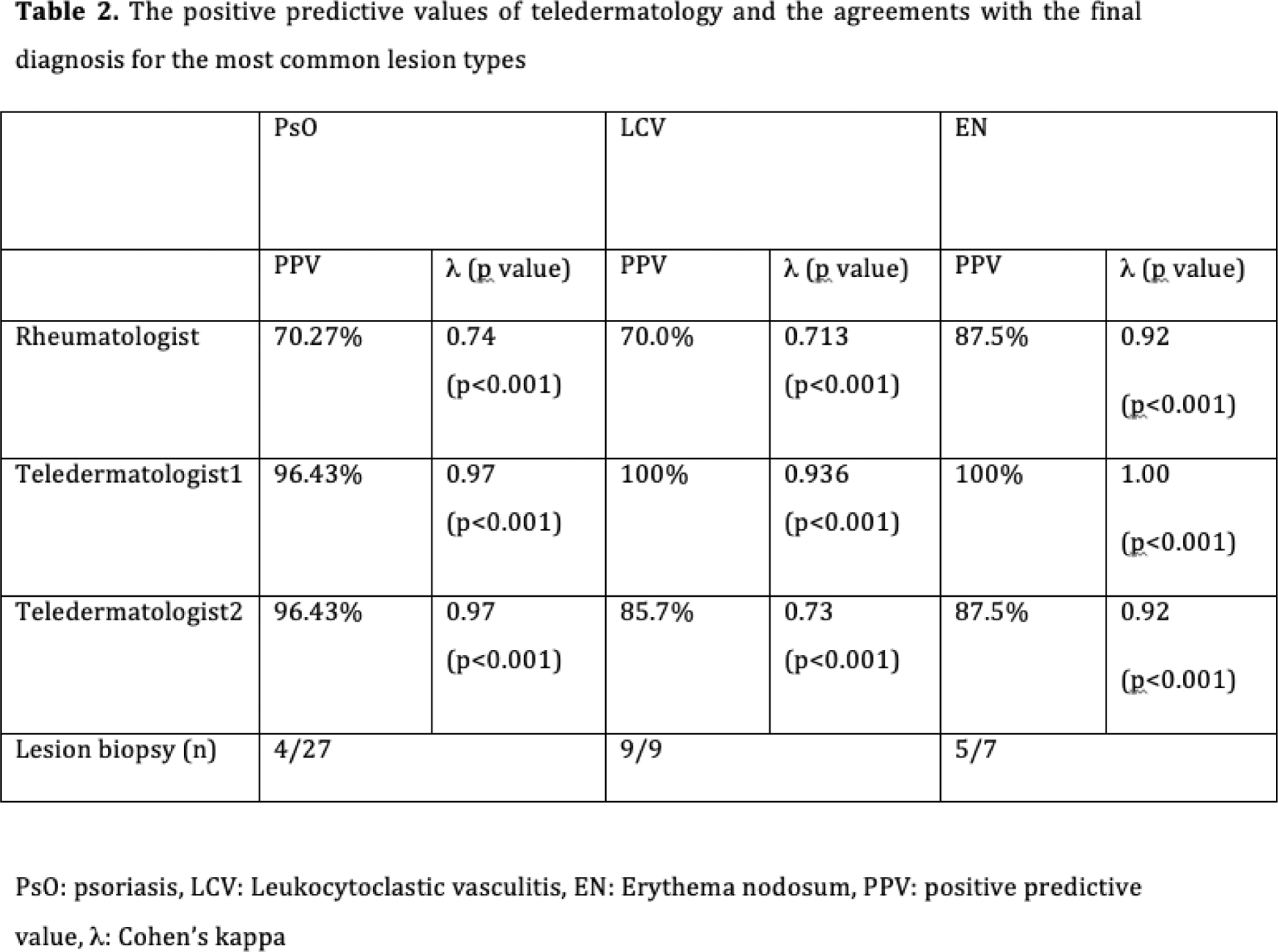
Results: The study included 113 rheumatology patients with skin lesions. When the definitive diagnoses were examined, it was found that psoriasis (PsO), leukocytoclastic vasculitis (LCV), and erythema nodosum (EN) were the most common skin lesions in rheumatic patients. The two teledermatologists were in perfect agreement; the rheumatologists were in substantial agreement with the final diagnosis. (Table 1). The inter-rater agreements of two teledermatologists were in substantial; the intra-rater agreement of the one teledermatologist was as in perfect agreement (Table 1). Rheumatologists’ positive predictive values for the most common lesions (PsO, LCV and EN) were shown to be lower than teledermatologists’ (Table 2).
Dermatologists diagnosed skin lesions in a particular group of patients without the need for further testing or biopsy (28.3% of all the patients). The majority of these lesions diagnosed clinically alone were PsO (16.8%), especially for cases of PsO found in predilection areas, plaque-type PsO, and accompanied by psoriatic nail involvement. On the other hand, skin biopsy was used to make a diagnosis in 40% of rheumatologic patients. The most common biopsied conditions were LCV, EN, PsO, SLE, and morphea. Dermatologists were shown to favor to make a biopsy 100% of vasculitis, 71% of EN, 14.8% of PsO, 100% of morphea, and 75% of SLE lesions.
Conclusion: TD could be used in rheumatological patients with skin lesions as a viable and reliable approach. Dermatologists who used TD had greater PPVs than rheumatologists. Thus, rheumatologists’ consultations with teledermatologists can strengthen their diagnosis. Dermatologists prefer FTF assessments and biopsies for lesions like vasculitis, while lesions like PsO will benefit best with TD in rheumatology practice.
REFERENCES: [1] Giavina-Bianchi M, Santos AP, Cordioli E. Teledermatology reduces dermatology referrals and improves access to specialists. EClinicalMedicine 2020;29-30:100641.
[2] Wong NWK, Towheed TE, Hopman W, Kirchhof MG (2018) Detection of dermatological abnormalities in the rheumatology clinic using a standardized screening exam. Int J Rheum Dis 21 (2):387-393.
[3] Samycia M, McCourt C, Shojania K, Au S (2016) Experiences From a Combined Dermatology and Rheumatology Clinic: A Retrospective Review. J Cutan Med Surg 20 (5):486-489.
Acknowledgements: NIL.
Disclosure of Interests: None declared.