

Background: Anti-SSA and -SSB antibodies are associated with neonatal lupus (NL), a condition that can affect fetuses/newborns of women with these circulating antibodies regardless of the presence of a systemic disease. However, data is inconclusive regarding the association of these antibodies and other obstetric complications.
Objectives: To describe maternal and perinatal outcomes of women with anti-SSA and SSB followed at a high-risk multidisciplinary pregnancy clinic and to address possible risk factors for adverse pregnancy outcomes (APO) in this population.
Methods: Retrospective observational study of patients followed at a tertiary hospital from 01/2009 to 05/2023. Included patients exhibited serum anti-SSA and/or anti-SSB determined by ELISA.
Results: A total of 103 pregnancies in 85 patients were included. There was 1 twin pregnancy. The median age at conception was 35.0 (IQR 31.0-37.0) years. Systemic Lupus Erythematosus (SLE) was the main diagnosis (n=36, 35.0%) followed by primary Sjögren syndrome (SSj) (n= 19, 18.4%). Concerning SLE patients, 7 had secondary antiphospholipid syndrome and 7 had secondary SSj. One patient with primary SSj had concomitant primary biliary cholangitis and another one concomitant mixed cryoglobulinemia. All pregnancies were anti-SSA positive - 69 (67.0%) anti-Ro52 and 86 (83.5%) anti-Ro60; 39 (37.9%) were anti-SSB positive.
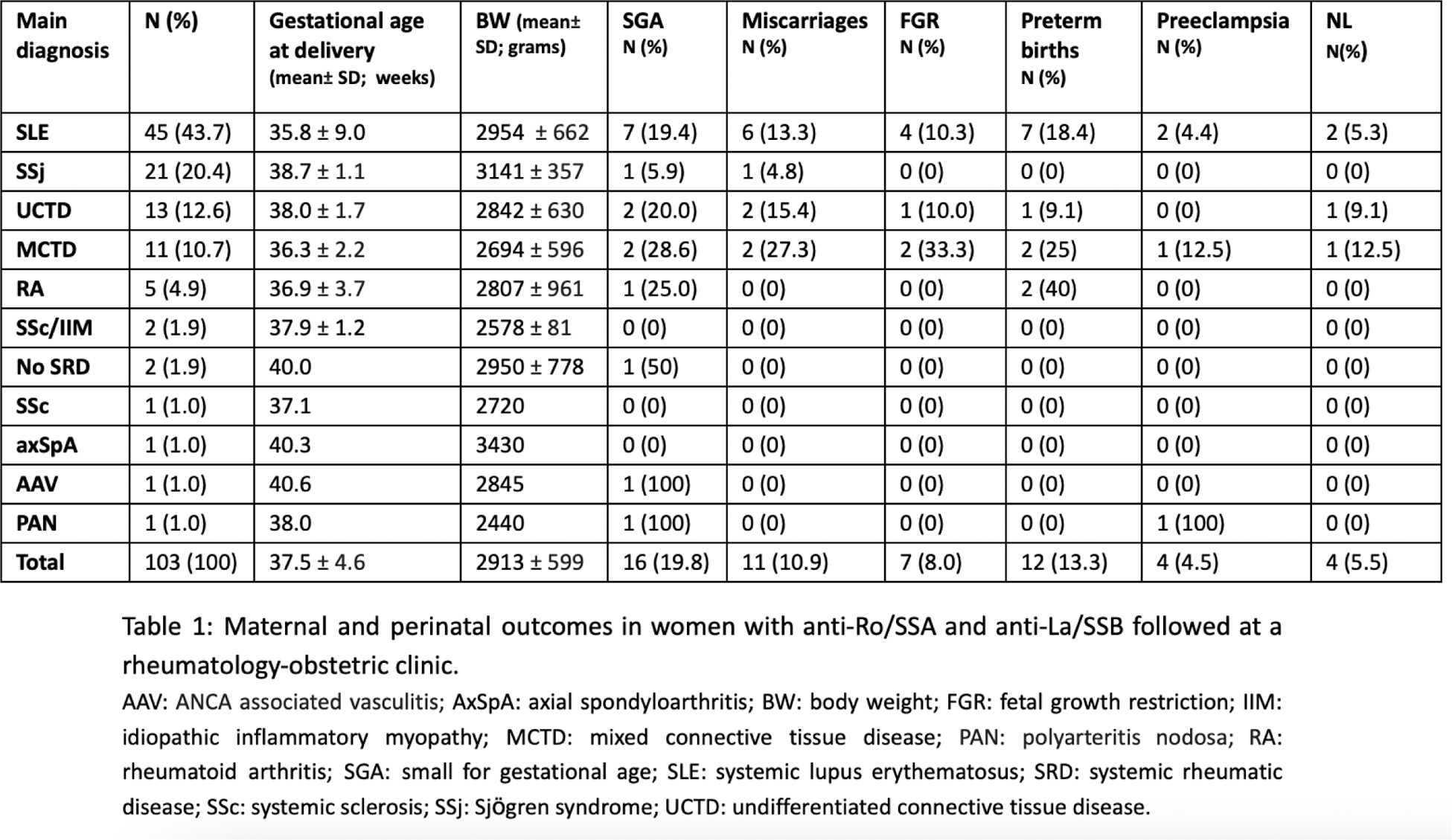
Table 1 summarizes clinical data. There was 1 stillbirth from a preterm labor, 1 medical termination of pregnancy because of severe malformations, and 11 (10.9%) miscarriages. Preeclampsia (PE) occurred in 4 (4.5%) pregnancies and preterm labor (PTL) in 12 (13.3%), 1 before the 34th week of gestation (WG). Fetal growth restriction (FGR) occurred in 7 (8.0%) cases and 16 (19.8%) newborns were small for gestational age. There were 4 (5.5%) cases of NL, expressed as skin rash (2) thrombocytopenia (1) and first degree congenital heart block (1). The latter successfully reverted after dexamethasone and IVIG treatment. The occurrence of PTL was associated with hypocomplementemia (p=.042). We found no correlation between anti SSA/SSB titers and the occurrence of APOs.
Conclusion: Only one case of 1 st degree heart block was recorded, reverting after treatment. PTL was associated with hypocomplementemia in our cohort. The majority of pregnant patients managed at our rheumatology-obstetric high-risk clinic had successful gestations. The risk of APO in positive anti-SSA/SSB pregnant women does not seem to be related with antibody titers. Further studies are needed to definitively establish if anti-SSA/SSB positive pregnant women are at higher risk of maternal and perinatal outcomes.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: Margarida Santos Faria: None declared, Ana Rita Lopes: None declared, Ana Teodósio Chícharo: None declared, Sofia C Barreira: None declared, Patrícia Martins AbbVie, Luísa Pinto: None declared, Mónica Rebelo: None declared, Ana Rita Araújo: None declared, Ana Rita Cruz-Machado: None declared, Susana Capela: None declared.