

Background: There is an increasing interest in the use of Artificial Intelligence (AI) in rheumatological care. Potential applications are the identification of subgroups of patients, prediction of diagnosis and response to treatment, automated image analysis and natural language processing to extract meaningful data from electronic health records. [1,2] Although the number of publications on the development and application of AI in rheumatology has increased sharply, implementation of AI applications in clinical practice remains scarce and evidence on the effectiveness of AI in improving patient outcomes is needed. [3] To ensure relevant applications of AI in rheumatology it is essential to involve end-users such as health care providers and explore their views.
Objectives: The objective of the current study was to explore the views of Dutch Rheumatology healthcare professionals on the use of AI in rheumatological care.
Methods: In September 2023, we conducted a survey at the Annual congress of the Dutch Society for Rheumatology (NVR) among the audience of a session on Artificial Intelligence. The session lasted 1,5 hour and included presentations covering the history, possibilities, benefits and risks of AI within rheumatology (1 hour) and subsequently a discussion with the audience (30 minutes). During the discussion, attendees were asked to answer (non-mandatory) multiple-choice questions on their smartphone using an interactive electronic platform (Wooclap). The questions addressed respondents’ characteristics (e.g. age, gender, function) and views on the use of AI within rheumatological care. Anonymous data was extracted from the platform and analysed.
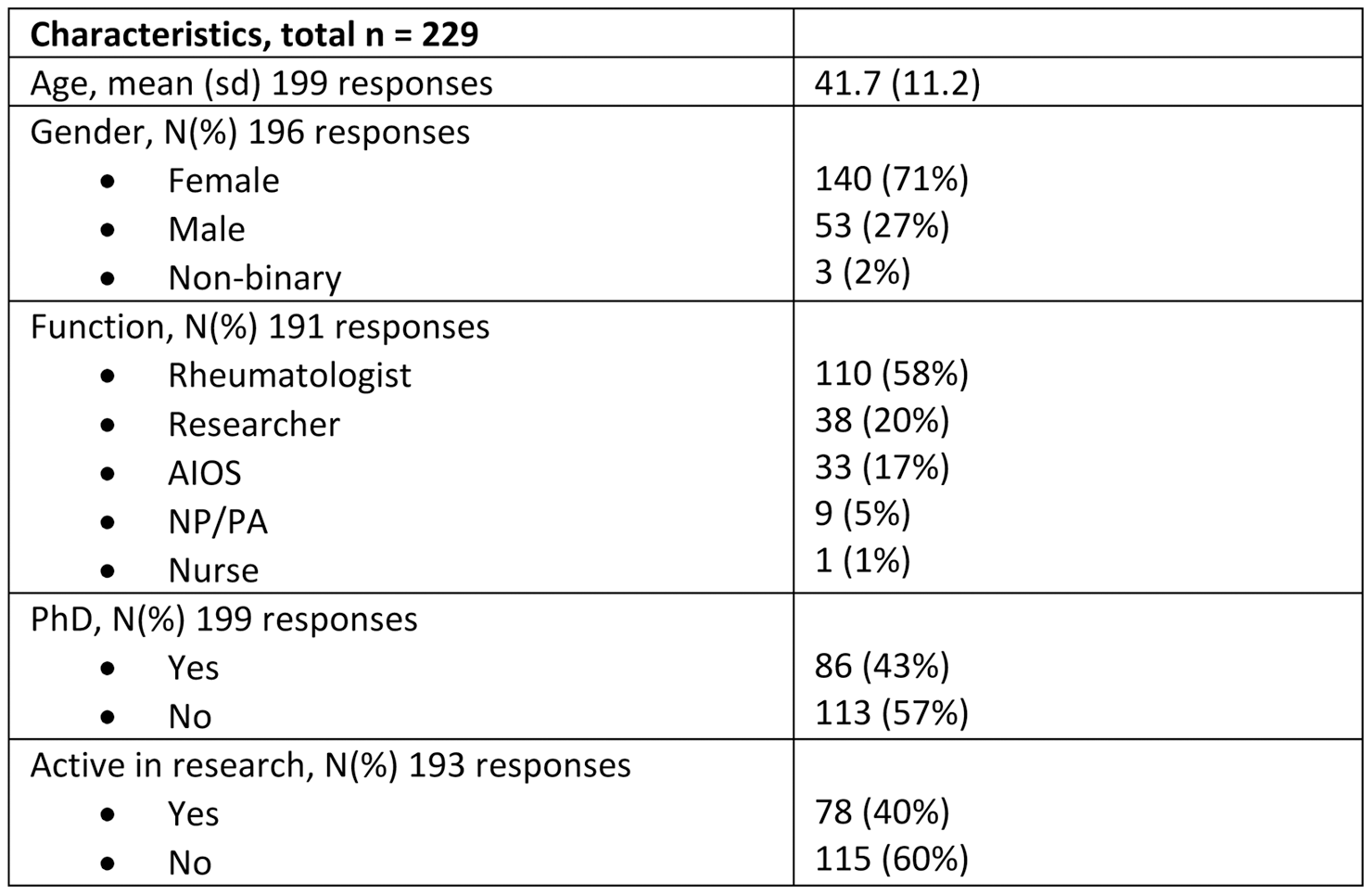
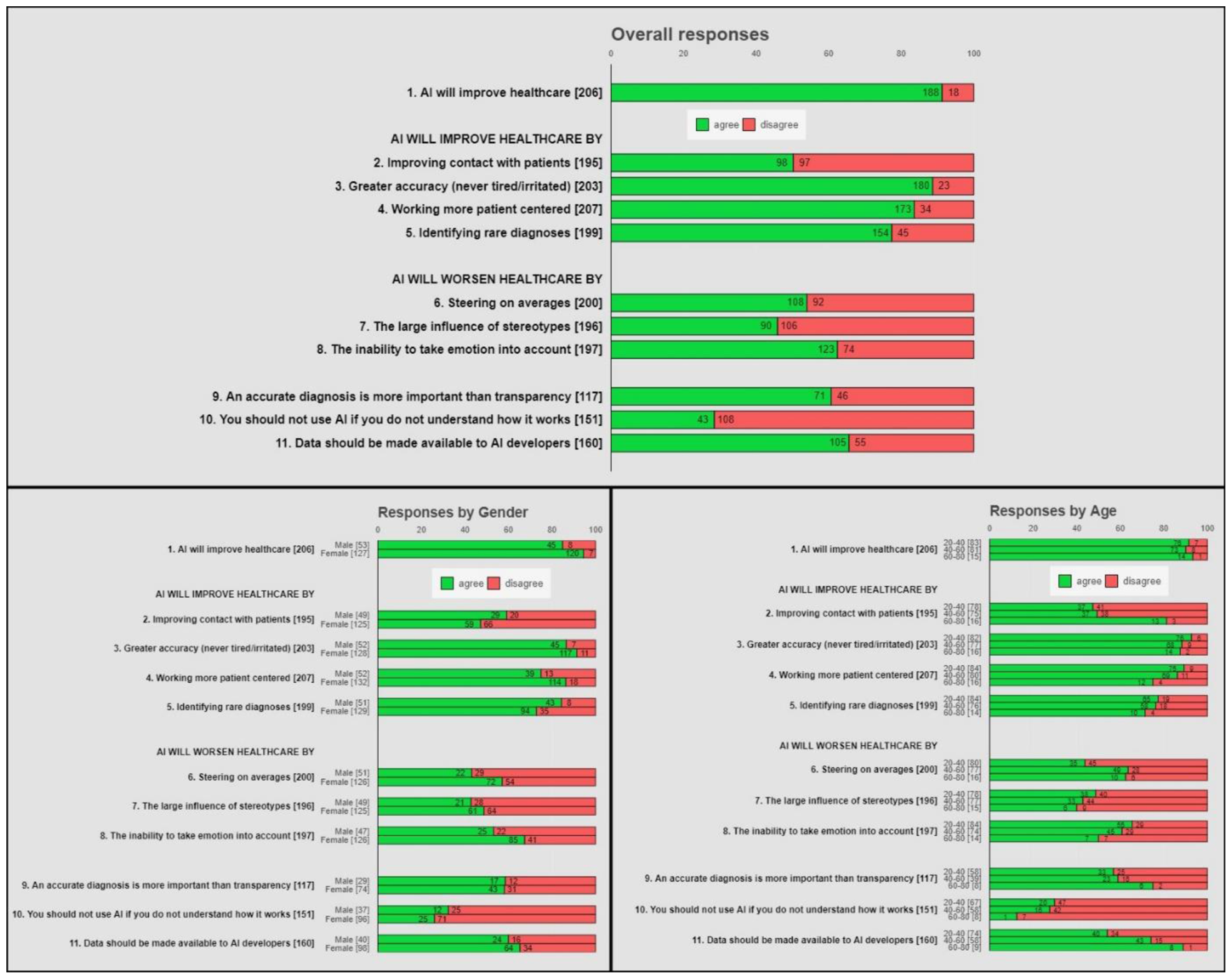
Results: 229 people (from 400 congress visitors) participated in our survey and completed at least one of the questions of the survey. Respondent characteristics are shown in Table 1. Seventy-one percent of respondents was female and 58% was rheumatologist. Responses (overall, by gender and by age group) to the statements are shown in Figure 1. Among 206 respondents, 188 (91%) agreed that use of AI would increase quality of care. Univariate logistic regression analysis indicated that gender was significantly associated with a positive response to this statement for females compared to males, 94% versus 84%, p=0.04. Other characteristics did not show a significant association with this statement. Due to a limited number of respondents, no multivariate analyses were performed. A large majority of respondents thought that AI would improve care by greater accuracy (89%), working more patient centred (84%) and the ability to identify rare diagnoses (77%). A majority of respondents indicated that the accuracy of a diagnosis was more important than insight in how this diagnosis was reached (61%), that not understanding AI should not be a barrier for using it (72%), and that health care data should be made available to AI developers as much as possible (66%). It was thought that rheumatologists could best use AI to take over or expand (part of) their tasks (54%) compared to rheumatologists in training (15%) and research nurses (31%). Excluding the 38 people who indicated to be a researcher did not impact results for most statements (changes ≤3%) except for statement 7 on the influence of stereotypes (41% agree) and statement 11 on making data available for AI developers (70% agree).
Conclusion: Dutch Rheumatology health care professionals are majorly positive about the potential of AI to improve rheumatological care given the limited current evidence. Females seem more positive than men and we did not find a difference based on age group. A majority agreed that accuracy is more important than explainability and that data should be made available to AI developers as much as possible. We cannot rule out selection bias, as people with more positive views on AI could be more inclined to attend a session on AI in rheumatology and answer our questions during the session. Findings might be influenced by the framing of questions and the limited time available for explanation.
REFERENCES: [1] Gossec et al. Ann Rheum Dis. 2020;79(1):69-76.
[2] Knevel R, Hügle T. RMD Open. 2022 Sep;8(2):e002401.
[3] Aristidou et al. Lancet. 2022;399(10325):620.
Table 1.
Acknowledgements: NIL.
Disclosure of Interests: None declared.