

Background: Patients diagnosed with Systemic Autoimmune Diseases (SAD) face distinct challenges during pregnancy potentially affecting maternal health and neonatal outcomes. Despite the well-known prominence of sleep and mental health disturbances in SAD and the vulnerability of mental health during pregnancy due to physiological, psychological, and hormonal changes, a significant gap persists in comprehending the prevalence, severity, and intricate interrelationships between sleep disturbances, anxiety, and depression symptoms in SAD during gestation.
Objectives: To investigate the prevalence of insomnia, anxiety, and depression symptoms in individuals with SAD during pregnancy. Additionally, this study evaluates the correlation between mood, anxiety, and insomnia, providing insights into the complex interrelationships among these factors.
Methods: This study assessed consecutive women during pregnancy diagnosed with SADs, including Connective Tissue Diseases (CTD), Inflammatory Arthritis (IA) and Systemic Vasculitis (SV) attending the pregnancy clinic of a tertiary referral center. Patients were evaluated through the Insomnia Severity Index (ISI), the State-Trait Anxiety Inventory (STAI Y1 and Y2), the Difficulties in Emotion Regulation Scale (DERS), the Mood Disorder Questionnaire (MDQ), and the Postpartum Depression Predictors Inventory-Revised (PDPI-R). Frequency analyses identified the prevalence of patients reporting significant symptoms (scores over the cut-point in the referred questionnaires). Non-parametric between group comparisons and correlations were used to evaluate the associations between clinical variables (diagnosis, pharmacological treatment, years between disease onset and pregnancy) and insomnia, mood, and anxiety symptoms with a significance level set at p-value <0.05.
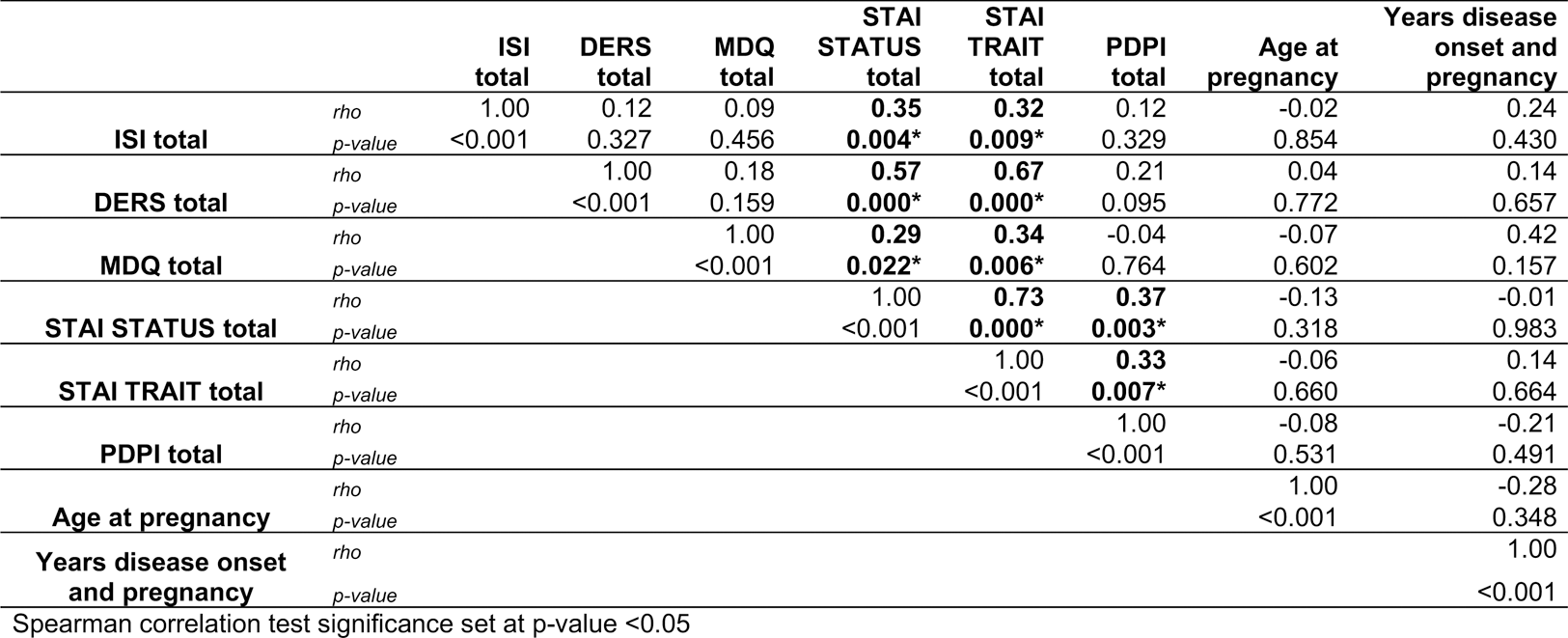
Results: Sixty-five patients were enrolled, with a mean age of 34.69 (±4.57) years and a mean disease duration of 9 (±5.10) years. Fifty patients (76.9%) were diagnosed with Connective Tissue Diseases (CTD), 20 (18.5%) with Inflammatory Arthritis (IA), and 3 (4.6%) with Systemic vasculitis (SV). Among the patients, 13 (22.8%) were receiving glucocorticoids (GCs), 33 (56.9%) hydroxychloroquine (HCQ), 9 (15.3%) traditional or biologic immunosuppressants (IS TRAD/BIO), and 29 (49.2%) anticoagulants or antiplatelet agents (ACT/APT). A high percentage of significant symptoms was found with prevalence rates of insomnia at 53.1%, anxiety symptoms at 45.3% (state) and 40.6% (trait), emotional regulation difficulties at 44.6%, significant mood disturbances at 10.8%, and a significant risk of postpartum depression in 6.2% of cases. Between-group comparisons based on diagnostic categories and pharmacological treatments revealed significant differences when patients were categorized according to hydroxychloroquine (HCQ) intake with significantly higher STAI-Y1 and PDPI-R scores in the group not consuming HCQ compared to the group consuming HCQ (p-value <0.05, see Table 1). Significant correlations were found between the STAI and ISI, MDQ and DERS scores (p <0.05, see Table 2).
Conclusion: This study sheds light on the underexplored psychological aspects of pregnancy in SAD, emphasizing the need for comprehensive mental health care in this population. Significant correlations between anxiety symptoms and mood, emotion regulation and insomnia suggest the necessity to further explore the role of anxiety as a trigger of mental health complications in this clinical population. The association emerged between the HCQ use and better scores in terms of anxiety symptoms and post-partum depression is intriguing. We could argue that HCQ may maintain better control over the underlying autoimmune condition thus influencing mental health outcomes during pregnancy. These are preliminary interpretations, and further research, including controlled studies and exploration of potential confounding factors, is needed to establish causation and understand the underlying mechanisms.
REFERENCES: NIL.
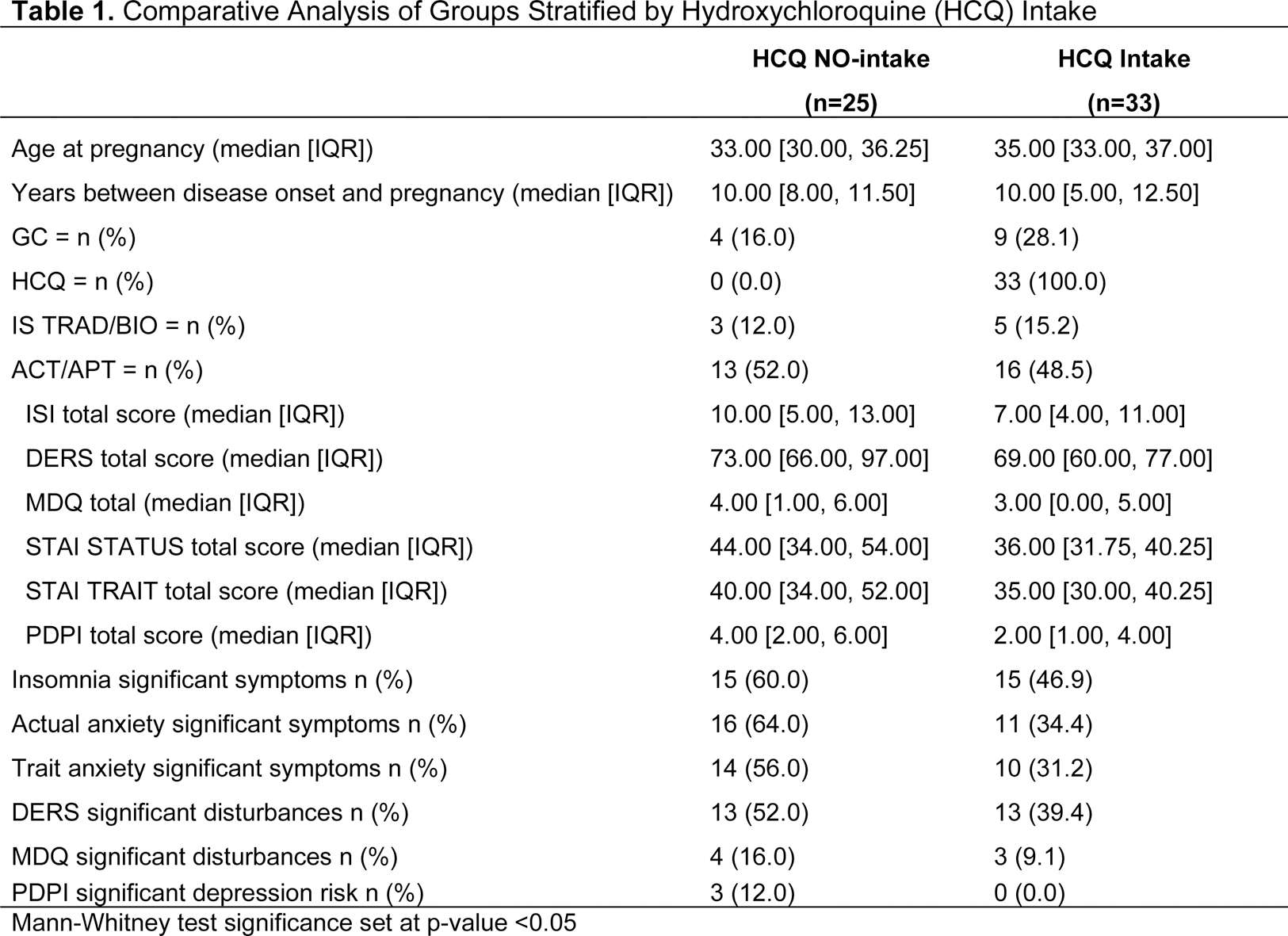
Table 2. Correlations between questionnaires total scores and age and disease duration in the overall sample
Acknowledgements: NIL.
Disclosure of Interests: None declared.