

Background: Flares of disease activity are common in rheumatoid arthritis (RA) and affect patients’ daily functioning, radiographic progression and disability. On the other end of the disease activity spectrum, remission remains the ultimate therapeutic goal. However, patients and rheumatologists often have different views on both concepts, which are challenging to define. Discrepancies may lead to different goals and expectations, complicating the therapeutic relationship and shared decision-making.
Objectives: To explore patients’ and rheumatologists’ perceptions on the concepts of flare and remission.
Methods: Patients with RA and rheumatologists were invited to take part in individual semi-structured interviews. Patients were recruited in the outpatient clinic of a tertiary centre and rheumatologists were invited via e-mail. Interviews took place in person, via telephone or via videocall. Participants were recruited until data saturation was achieved, defined as no new data emerging from the last 3 interviews. Interviews were audio recorded, transcribed verbatim and a thematic analysis was conducted guided by the principles of the constant comparative method. Two patient research partners were involved in the study design and provided feedback on the identified themes.
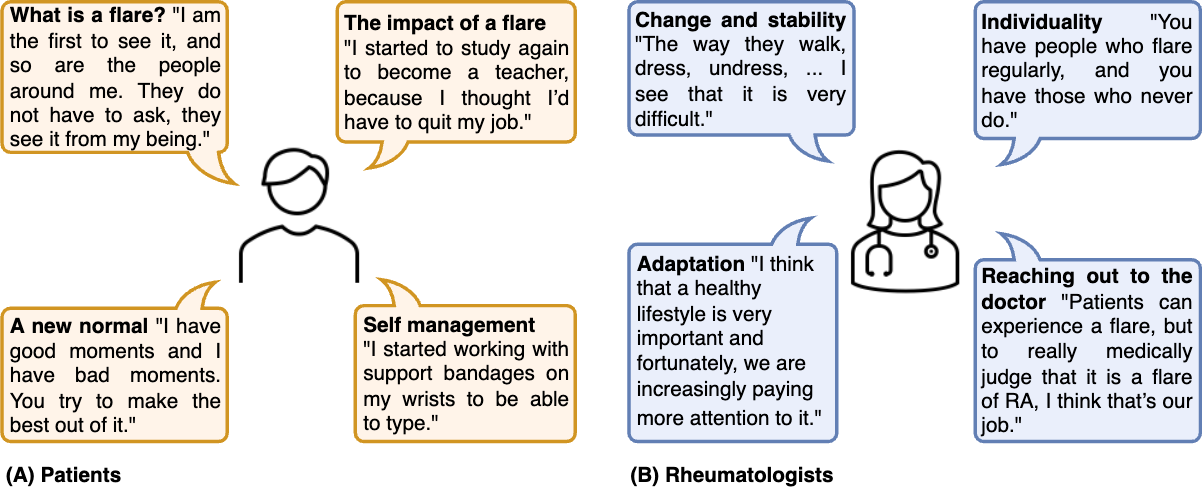
Results: 13 patients and 10 rheumatologists were interviewed (Table 1). Among patients, four themes emerged (Figure 1A): (1) What is a flare? , where patients expressed they were capable of identifying flares themselves, and rheumatologists were sought for confirmation and help. (2) The impact of a flare , where an increase in pain was identified to be a hallmark of flares, while fatigue, although highly disabling, appeared more continuously present and seemed less suitable to identify flares with. Patients emphasised the impact of flares on social roles and psychological wellbeing. (3) A new normal , where true remission was seen as being pain-free and returning to normality, the latter requiring a process of acceptance and adaptation. (4) Self-management , where patients highlighted the importance of skills to prevent and cope with flares, mentioning the value of rest and a positive mindset.
Among rheumatologists, four themes emerged (Figure 1B): (A) Change and stability , where rheumatologists identified flares as changes in disease activity leading to changes in function and behaviour, while remission reflected stability in disease activity and quality of life. (B) Individuality , where the individual nature of flares and remission across patients was noted. The importance of knowing a patient’s history was mentioned, as some patients contacted rheumatologists more easily than others. (C) Adaptation , where the beneficial effects of education and self-management skills were mentioned to identify, manage and prevent flares. (D) Reaching out to the doctor , where rheumatologists described the help seeking behaviour of patients. Rheumatologists did not unanimously agree whether patients were capable of identifying flares, bringing up that patients sometimes wrongly linked unrelated symptoms to flares. Nonetheless, the importance of shared decision-making for managing disease burden was emphasised.
Conclusion: While patients felt confident in their ability to recognise flares, some rheumatologists disagreed, mentioning that unrelated symptoms are sometimes wrongly attributed to flares. Remission was defined more strictly by patients as being pain-free and returning to normality, while rheumatologists described remission in terms of stability. Both patients and rheumatologists acknowledged the impact of a flare in terms of symptoms and psychosocial consequences, and shared decision-making was thought to be vital in managing disease burden.
REFERENCES: NIL.
Table 1. Participant characteristics.
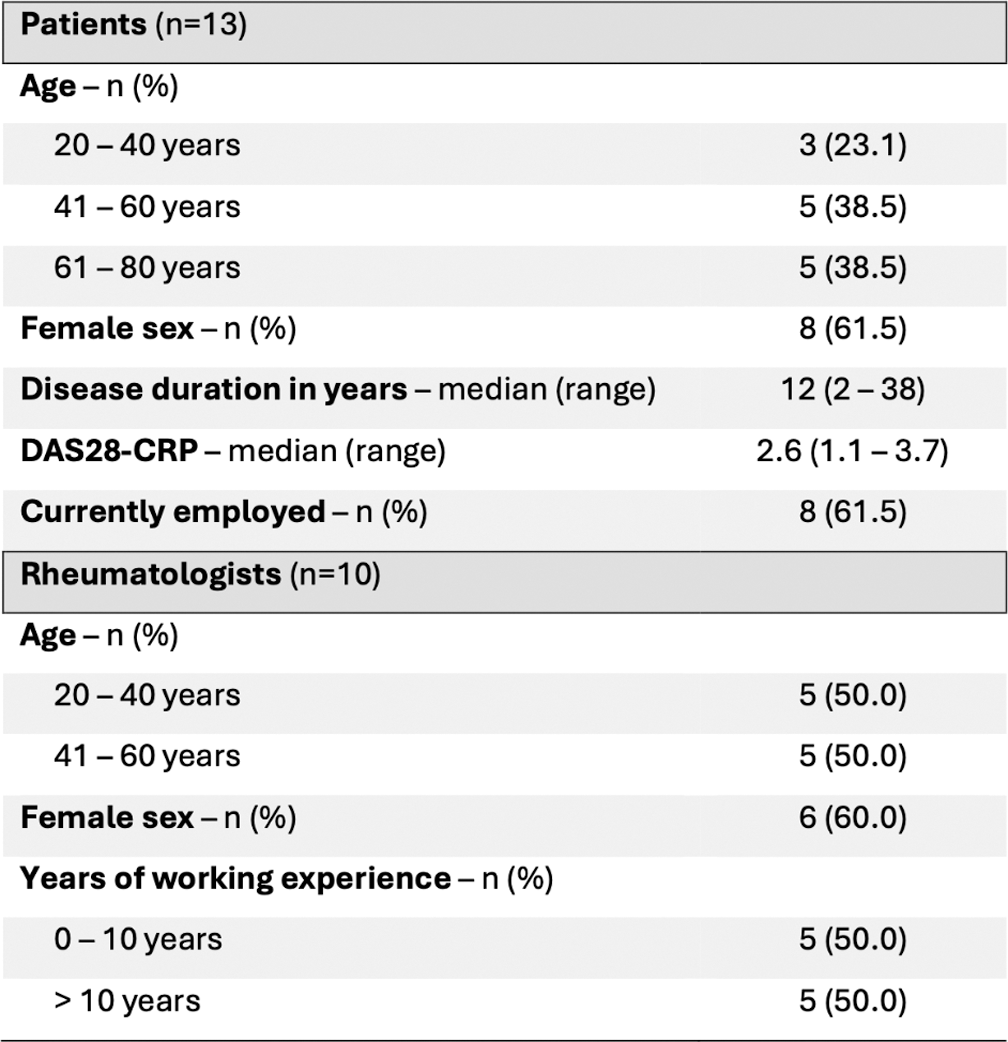
DAS28-CRP: Disease Activity Score in 28 joints – C-reactive protein
Themes identified among (A) patients and (B) rheumatologists, illustrated with quotes.
Acknowledgements: NIL.
Disclosure of Interests: None declared.