

Background: Systemic Lupus Erythematosus (SLE) is a complex autoimmune disease with diverse symptoms and multisystemic manifestations. [1] Reducing exacerbations (flares), often leading to hospitalization, remains a challenge in the care of patients with SLE. [2]
Objectives: This study aims to understand the association of validated Patient Reported Outcomes (PROs) such as Systemic Lupus Activity Questionnaire (SLAQ) and Brief Index of Lupus Damage (BILD) to hospitalization.
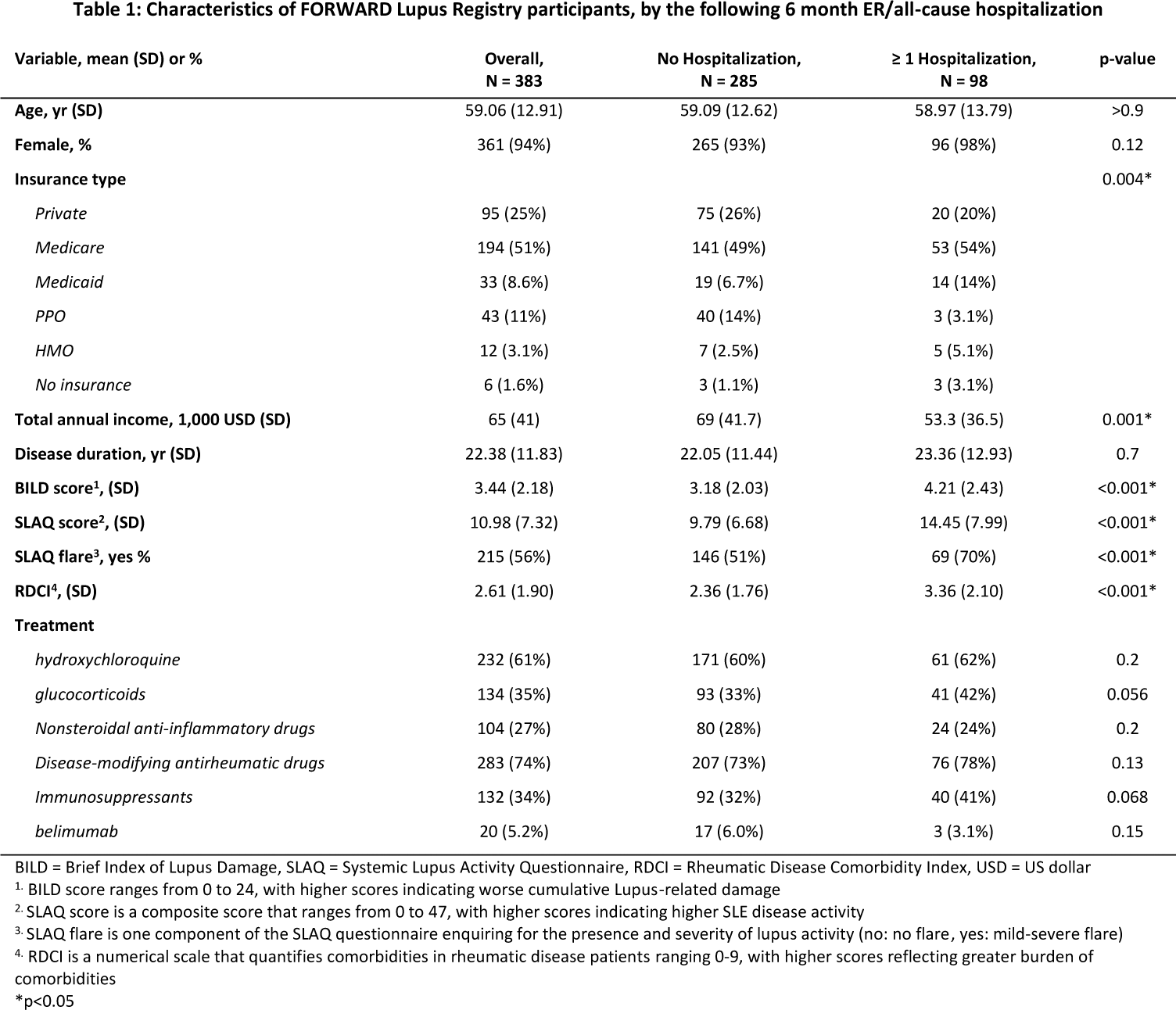
Methods: The FORWARD Lupus Registry (FLR) is a US longitudinal patient-reported registry, collected through FORWARD, The National Databank for Rheumatic Diseases. [3] Patients with at least two consecutive FLR biannual surveys who completed age, sex, SLAQ, SLAQ flare component, and BILD at baseline and hospitalization (emergency room (ER) and/or all-cause hospitalization) at their consecutive biannual survey were included. Descriptive analyses were conducted on socio-demographics, disease characteristics, Rheumatic Disease Comorbidity Index (RDCI) [4] , and treatment at baseline, stratified by hospitalization (0 or 1+). Group differences were assessed using t-test and Chi-square tests (or Fisher’s exact test), when appropriate. Three distinct multivariate logistic regression models examined the relationship of prior SLAQ score, SLAQ flare component, BILD score to hospitalization, individually, and adjusting for potential confounders (age, sex, insurance type, total annual income, RDCI, and treatments).
Results: Out of 383 FLR patients, 98 (25.6%) had an ER visit or all-cause hospitalization in their consecutive biannual survey (22.7% ER, 13.8% all cause-hospitalization, 11% both from the total). The mean BILD and SLAQ score were significantly higher in the ≥ 1 Hospitalization group (BILD: 4.21 (SD 2.43) vs 3.18 (SD 2.03), p<0.001; SLAQ: 14.45 (SD 7.99) vs 9.79 (SD 6.68), p <0.001), with more flares reported through the SLAQ flare component (70% vs 51%, p<0.001) (Table 1). SLAQ score and SLAQ flare component were significant predictors of hospitalization in their respective models (OR=1.07; 95%CI: 1.02-1.11, OR=2.26; 95%CI: 1.24-4.14), while BILD score showed a similar trend but was not statistically significant (OR=1.10; 95%CI: 0.96-1.27). RDCI was a statistically significant predictor of hospitalization in all three multivariate models, increasing the odds of hospitalization (OR=1.33, 95%CI 1.15-1.54, OR=1.25, 95%CI 1.07-1.46, OR=1.29; 95%CI: 1.11-1.51).
Conclusion: SLE patients with higher SLAQ score, or having any flare reported by the SLAQ flare component irrespective of the severity are at higher risk of hospitalization. Patient-reported disease activity should be considered in clinical setting for the evaluation of SLE patients and the management of lupus to minimize frequency of flares.
REFERENCES: [1] Adamichou C, Bertsias G. Flares in systemic lupus erythematosus: diagnosis, risk factors and preventive strategies. Mediterr J Rheumatol. 2017 Mar 28;28(1):4-12. doi: 10.31138/mjr.28.1.4. PMID: 32185248; PMCID: PMC7045928.
[2] Katz P, Nelson WW, Daly RP, Topf L, Connolly-Strong E, Reed ML. Patient-Reported Lupus Flare Symptoms Are Associated with Worsened Patient Outcomes and Increased Economic Burden. J Manag Care Spec Pharm. 2020 Mar;26(3):275-283. doi: 10.18553/jmcp.2020.26.3.275. PMID: 32105178; PMCID: PMC10390967.
[3] Frederick Wolfe, Kaleb Michaud, The National Data Bank for rheumatic diseases: a multi-registry rheumatic disease data bank,
Rheumatology
, Volume 50, Issue 1, January 2011, Pages 16–24,
[4] England, B. R., Sayles, H., Mikuls, T. R., Johnson, D. S., & Michaud, K. (2015). Validation of the Rheumatic Disease Comorbidity Index. Arthritis Care & Research, 67(6), 865–872.
Acknowledgements: NIL.
Disclosure of Interests: Minjee Park Former employee of GSK, Employee of Alira Health, Sofia Pedro Employee of FORWARD the National Databank of Rheumatic Diseases, Jean-Francois Ricci Former employee of GSK and Novartis, Employee of Alira Health, Kaleb Michaud Employee of FORWARD the National Databank of Rheumatic Diseases, Patricia Katz: None declared.